Abstract
We present a 50-year-old woman with left adrenal sarcoidosis. She visited our hospital for right upper quadrant discomfort; she was then evaluated for right upper quadrant discomfort. She had no abnormal findings in the laboratory examination, including hormone study, but a mass was detected at left adrenal gland, incidentally. Initially, we thought the mass as nonfunction adrenal adenoma. After she had undergone laparoscopic left adrenalectomy, she was diagnosed with left adrenal sarcoidosis from her histological findings. Adrenal sarcoidosis is a very rare disease. This case provides insight to the experience of left adrenal sarcoidosis.
Sarcoidosis is an idiopathic granulomatous disease. It usually affects the lung but may involve any organ. However, endocrine involvement is uncommon especially in adrenal gland. We report the case of sarcoidosis of left adrenal gland and inquiry of document.
A 50-year-old woman visited our hospital for complaining right upper abdominal pain. On physical examination, there were no abdominal findings on her body. She seemed to have a good general condition. She didn't appeal any discomfort on her ordinary activity. Her laboratory findings showed that a white blood cell count was 6,830/mm3 with 69% segment neutrophil. Liver and renal functions were within normal limits. Her serum calcium level was within normal limit. The serum angiotensin-converting enzyme level was 34.7 u/ml (18~67). Her adrenal hormone study showed normal range of count; VMA 1.94 mg/day (<7.0), 24-hour urinary excretion of 17-OHCS and 17-KS were 6.54 mg/day (2~12) and 4.68 mg/day (6~15). Plasma concentration of ACTH, cortisol and DHEAS were 11.6 pg/ml (6~30), 185.6µg/day (>120) and 71µg/dl (35~430) respectively.
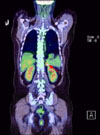
Her chest radiologic finding showed definitely non-abnormality (Fig. 1). Computed tomography of her abdomen revealed multi-nodular thickening of left adrenal gland (less than 2×1.4 cm), suggesting an adrenal adenoma or malignant lesion and several prominent paraaortic lymphnodes (Fig. 2). Computed tomography of her chest revealed an about 0.9 cm, relatively well-defined, non-calcified nodule at superior segment of left lower lobe, near the interlobar fissure. PET CT revealed an about 2×1.4 cm sized mass with increased FDG uptake (mSUV of 7.9) at left adrenal gland, suggesting malignant tumor at left adrenal gland (Fig. 3).
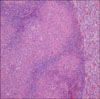
Then, we planed laparoscopic adrenalectomy for an exact diagnosis. She underwent laparoscopic left adrenalectomy and the gross finding of the adrenal mass was yellow-colored tissue measuring 5.5×3.2×2.2 cm which had irregular margin and rubbery contexture (Fig. 4). There was no invasion to adjacent organ and no enlarged lymph node. The histologic finding of the operated specimen showed left adrenal sarcoidosis, there are non-caseating granulomas mainly composed of epithelioid cell, with scattered Langhans' giant cells and lymphocytes (Fig. 5). She was discharged without any complications after 7 days of hospitalization.
Sarcoidosis is a multisystem protean disorder, characterized histologically by the presence of non-caseating epithelioid-cell granulomas in affected tissue.(1) Its cause is still unknown and its treatment and prognosis are uncertain. The lung is the most common organ affected with sarcoidosis. However, the disease may involve any part of the body,(2) including endocrine organ: hypothalamus, hypophysis, thyroid gland, parathyroid gland, adrenal gland and calcium metabolism disorder.(3) Onset is most common between the ages of 20 and 40 years, although sarcoidosis is occasionally reported in childhood and in the elderly. Sarcoidosis may run not only a chronic course but also a transient course.(1) Extrapulmonary sarcoidosis may be more frequent in females in the study of sarcoidosis prevalence in a health maintenance organization database.(4) Families with two or more first-degree relatives affected with sarcoidosis are a common occurrence.(5)
The diagnosis of sarcoidosis requires compatible clinical findings, histologic demonstration of non-caseating granulomas, and exclusion of alternative diseases. For evaluation, blood should be obtained to evaluate liver and renal functions. A complete blood count may suggest bone marrow or splenic involvement. A urinalysis may suggest nephrolithiasis if hematuria is detected. A tuberculin skin test should be performed for consideration of tuberculosis. An ophthalmologic examination should be performed to evaluate the patient for sarcoidosis involvement of the eye. An electrocardiogram should be done as a screening test for cardiac involvement.(2)
Therapy is not mandated for sarcoidosis because the disease may remit spontaneously, so asymptomatic patients should not be treated with the exception of those with involvement of eye and possibly heart and central nervous system; indication of therapy potential dangerous disease including cardiac sarcoidosis, neurosarcoidosis, hypercalcemia unresponsive to dietary measures, any ocular involvement, and other life-threatening conditions. Therapy should also be considered when the disease is progressive. Therapy for extrapulmonary sarcoidosis must be individualized. The basic approach should be to reduce the corticosteroid dose to the lowest effective dose with the ultimate plan on discontinuation. Methotrexate, hydroxychloroquine are the most studied alternative medications, and they are usually used as corticosteroid sparing agents. Methotrexate is most useful for pulmonary, eye, skin, and joint sarcoidosis. Hydroxychloroquine is most effective for skin, neurosarcoidosis, and calcium disorders from sarcoidosis. Azathioprine, leflunomide, mycophenolate monocycline, doxycycline and cyclophosphamide have been useful in small series.(2)
Sarcoidosis in adrenal glands is rarely reported. The functional status of the adrenal gland in patients with sarcoidosis has nearly always been normal when evaluated after stimulation with exogenous ACTH, with the exception of patients with secondary adrenal failure due to hypothalamic-pituitary infiltration by sarcoid granulomas.(6) Sarcoidosis of adrenal cortex may cause primary insufficiency of the suprarenal gland due to be replaced by dense fibrosis. The secondary insufficiency of the suprarenal gland is caused by hypothalamic and pituitary sarcoidosis.(3) Sarcoidosis of the adrenal gland has also been described as leading to an adrenal crisis and death.(7,8)
In conclusion, this report shows a rare case of adrenal sarcoidosis. This case was detected incidentally and doesn't have any abnormal findings on physical examination and laboratory test. This report can be an example that sarcoidosis which can involve any organ in the body including adrenal gland and the patient can be asymptomatic.
Figures and Tables
Fig. 2
Abdominal CT. There is multi-nodular thickening of left adrenal gland (less than 2×1.4 cm) suggesting adrenal adenoma or malignant lesion.

References
1. Porter N, Beynon HL, Randeva HS. Endocrine and reproductive manifestations of sarcoidosis. QJM. 2003. 96:553–561.
2. Judson MA. Sarcoidosis: clinical presentation, diagnosis, and approach to treatment. Am J Med Sci. 2008. 335:26–33.
3. Gostiljac DM, Dordević PB, Maric-zivković J, Canović F. Sarcoidosis localized in endocrine glands. Med Pregl. 2005. 58:Suppl 1. 25–29.
4. Baughman RP, Teirstein AS, Judson MA, Rossman MD, Yeager H Jr, Bresnitz EA, et al. Clinical characteristics of patients in a case control study of sarcoidosis. Am J Respir Crit Care Med. 2001. 164:1885–1889.
5. Rybicki BA, Iannuzzi MC, Frederick MM, Thompson BW, Rossman MD, Bresnitz EA, et al. Familial aggregation of sarcoidosis. A case-control etiologic study of sarcoidosis (ACCESS). Am J Respir Crit Care Med. 2001. 164:2085–2091.
6. Vesely DL, Maldonodo A, Levey GS. Partial hypopituitarism and possible hypothalamic involvement in sarcoidosis: report of a case and review of the literature. Am J Med. 1977. 62:425–431.
7. Karlish AJ, MacGregor GA. Sarcoidosis, thyroiditis, and Addison's disease. Lancet. 1970. 2:330–333.
8. Mayock RL, Bertrand P, Morrison CE, Scott JH. Manifestations of sarcoidosis. Analysis of 145 patients, with a review of nine series selected from the literature. Am J Med. 1963. 35:67–89.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download