Abstract
Purpose
The main treatment modality of peripheral arterial occlusive disease (PAOD) of the lower extremities has shifted from traditional bypass surgery (BS) to a less invasive endovascular intervention (EI), but there is still conflicting data about the differences in long-term patency between the two modalities The purpose of this study was to analyze restenosis rates of femoral EI and to compare both anatomical and functional results between EI and femorodistal BS.
Methods
Between July 2003 and June 2009, 88 limbs (61 patients) and 47 limbs (43 patients) with femoral artery PAOD were treated with EI and BS, respectively. A retrospective analysis of prospectively collected data was performed by reviewing medical records, radiologic images and noninvasive vascular studies. Patient demographics and risk factors were analyzed. Technical outcomes such as restenosis rates, patency rates and functional outcomes using modified questionnaires were evaluated.
Results
The restenosis rates for EI at 6 months, 1 year, 2 years and 3 years were 10.4%, 20.1%, 41.1% and 52.7%, respectively, and the mean restenosis duration was 36.5±3.24 months. Comparison of patency rates between EI and BS showed no significant difference (P=0.204) in TASC C and D lesions. Functional outcome analysis showed that both EI and BS improved functional status after treatment, and comparison between the two groups showed that BS had a better functional improvement than EI (P=0.010).
The incidence of peripheral arterial occlusive disease (PAOD) is increasing in most developed countries, mainly due to increasing proportion of the elderly population. Therefore, improved quality of life and concern for better health have brought about an increase in the diagnosis rate of PAOD.(1,2) The increasing prevalence of diabetes, cardiovascular and cerebrovascular diseases are also influential. However PAOD is still an underdiagnosed and undertreated disease, and leads to major socio-economic losses in terms of medical and social resources.(3) Infrainguinal, lower extremity PAOD can lead to walking impairment, ranging from intermittent claudication to critical limb ischemia (resting pain with or without tissue loss).
Traditionally, femorodistal bypass surgery (BS) for the stenotic or occluded artery was the gold standard of treatment for PAOD, mainly due to better long-term patency rates.(4,5) Endovascular intervention (EI), on the other hand, was strictly restricted to high-risk surgical patients. However BS has the disadvantage of having higher morbidity and mortality rates compared to other less invasive procedures.(6) Furthermore, technological advances have extended the use of the less invasive EI as first-line treatment.(7-11) The Trans Atlantic Inter-Society Consensus II (TASC II) for the management of PAOD recommends the use of EI as first-line treatment for the less severe TASC A and B lesions, while BS is still preferred for the severer TASC C and D lesions.(1)
The success rates of both EI and BS are measured by determining the anatomical patency. However increased patency does not always necessarily correlate with improved functional outcome, and the functional outcome between EI and BS may differ even if the patency of both procedures are the same. The aim of this study was to analyze restenosis rates of femoral EI at our institution and to compare both anatomical and functional results between EI and BS, mainly for TASC C and D lesions.
Between July 2003 and June 2009, EI for femoral artery PAOD was performed in 88 limbs from 61 patients and BS was performed in 47 limbs from 43 patients at our institution. For both groups, the medical records, radiologic studies and non-invasive tests were retrospectively reviewed. Patient demographics were recorded and risk factors related to PAOD such as diabetes mellitus (DM), hypertension, cardiovascular and cerebrovascular diseases, chronic renal failure were analyzed. The initial presenting symptom was classified as either intermittent claudication or resting pain/ulceration. The radiologic studies included diagnostic angiography, computed tomography angiography and duplex ultrasonography, and the severity of the lesions were categorized according to the TASC II Criteria based on these studies. As non-invasive testing, ankle-brachial index (ABI) tests were performed both preoperatively and postoperatively.
EI included all cases of balloon angioplasty, endovascular stenting or subintimal angioplasty. BS included femoropopliteal or femoro-tibial bypasses, using autogenous saphenous veins in 28 cases and prosthetic grafts in 19 cases.
Functional outcome for both groups was assessed using two standardized questionnaires: the Walking Impairment Questionnaire (WIQ) and the 36-question Short Form Health Survey (SF-36).(12-14) The WIQ for PAOD determines the walking ability of patients by measuring walking distance, walking speed and stair climbing. For each parameter, the degree of difficulty is given a score of 0 (inability to walk) to 3 (no difficulty) and each score is multiplied by the different distances, speeds or stairs. The products are then summed and divided by the maximum possible score to obtain a percentage score.(12) The SF-36 measures functional ability, both physical and emotional. Physical health (PH) is subdivided into 4 categories: physical functioning, role-physical, bodily pain and general health. Emotional health is also subdivided into 4 categories: vitality, social functioning, role emotional and mental health. Scoring is done by using a 0~100 scale, 100 being the highest possible score and therefore having the best functional capacity.(13) However in our study, we only analyzed PH, and scoring was done from 0 to 50. Both the WIQ and SF-36 (PH only) were performed retrospectively by a telephone survey before and after treatment.
In our study, restenosis after EI was defined as a stenosis of more than 50% on radiologic examination or a decrease in ABI of more than 0.20 with accompanying symptomatic aggravation in either case. Patency for both EI and BS was defined as the interval from the time of intervention or surgery until femoral artery occlusion.
Restenosis rates for EI and patency rates for both EI and BS were compared using the Kaplan-Meier survival analysis. The log-rank method was used for univariate analysis, and the Cox proportional hazard analysis for multivariate analysis, in accordance with reporting standards.(15, 16) Analysis of functional outcome was done using a paired t-test to determine significant changes before and after treatment, and a student t-test was used to compare functional outcome between EI and BS. All analyses were conducted using SPSS 15.0 for Windows (SPSS Inc., Chicago, IL, USA) and a P-value<0.05 was defined as statistically significant.
Demographic data are shown in Table 1. Both EI and BS showed a male predominance (77% for EI, 91% for BS). Hypertension and DM were the most common risk factors. According to initial symptom, there was no difference between claudication and critical limb ischemia (resting pain/ulceration) in the EI group (52% vs. 48%) but critical limb ischemia was more common in the BS group. The proportion of TASC A, B, C and D was 24%, 37%, 31% and 8% for EI and 0%, 15%, 32% and 53% for BS, respectively. There was a predominance of TASC A and B lesions in the EI group, and TASC C and D lesions in the BS group.
In the EI group, there were 9 deaths and 13 follow-up losses at the end of the study period with an overall follow-up rate of 85%, while in the BS group, there were 13 deaths and 16 follow-up losses, overall follow-up rate being 66%.
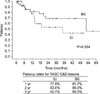
The restenosis rates for the EI group at 6 months, 1 year, 2 years and 3 years were 10.4%, 20.1%, 41.1% and 52.7% respectively and the mean restenosis duration was 36.5±3.24 months (Fig. 1). EI restenosis rates for TASC A, B, C and D showed a tendency for the severe lesions to have higher restenosis rates, although there was no statistical significance (Fig. 2). EI patency rates according to initial symptom showed no statistically significant difference (P=0.415) (figure not shown).
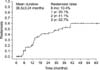
On the univariate analysis of variables affecting primary EI patency, only male gender (P<0.01) and the presence of DM (P=0.014) were statistically significant. However on the multivariate analysis, male gender (P=0.05), DM (P=0.01) and TASC D (P=0.04) were statistically significant. Patency rates for BS were analyzed according to the TASC II criteria, initial symptom, distal anastomosis site and graft type (figures not shown). Since there were no TASC A lesions in the BS group, TASC A and B were grouped together and TASC C and D were also grouped for comparison. There was a tendency for TASC C and D lesions to have a lower patency rate than TASC A and B lesions (80.0% vs. 69.0% at 3 years), but this tendency was not statistically significant (P=0.745) (figure not shown). Also initial symptom, distal anastomosis site and graft type showed no difference. Finally, patency rates for TASC C and D lesions were compared between EI and BS. One, 2, 3-year patency rates for TASC C and D lesions were 86.1%, 70.9%, 56.9% for EI and 84.4%, 70.6%, 70.6% for BS (Fig. 3). BS showed better patency rates than EI in the long-term with no statistically significant difference (P=0.204) (Tables 2, 3).
Functional outcome was assessed by both the WIQ and the SF-36 (PH only) (Table 4). Both the WIQ and the SF-36 (PH only) showed that functional outcome was much better after treatment in both EI and BS groups than before treatment (all P-values <0.05). In order to assess which treatment modality had better functional outcome, the differences in scores before and after treatment were calculated for both the WIQ and the SF-36 (PH only) and were statistically analyzed (Table 5). Overall, the differences in scores before and after treatment were higher for BS than for EI, and the SF-36 (PH only) proved this difference was statistically significant (P=0.010) but in the case of the WIQ, it was not significantly different (P=0.145).
The purpose of this study was to analyze the results of treatment for PAOD at our institution. Treatment methods included the traditional femorodistal BS and the less invasive EI. The results were analyzed in terms of both anatomical and functional improvement. The key point of this study was that the functional outcomes were analyzed because anatomical improvements in terms of increased patency on radiologic studies do not always correlate with an increase in function of the patient. After all, the main purpose of treatment is the symptomatic improvement and therefore the increased functional ability of the patient.
The TASC II Working Group provided a treatment guideline according to the severity of the lesion.(1) This guideline recommended that TASC A and B lesions should be treated using EI as first choice. On the other hand, TASC C and D lesions should be considered for BS as first-line treatment. Our data showed that our institution did follow this guideline when considering the choice of treatment for all patients. Out of the 88 lesions in which EI was performed, 61% were either TASC A or B, and only 8% were TASC D. These TASC D patients who underwent EI were surgically high-risk patients, with higher risks than benefits if surgery was to be performed. In the case of BS, there were no patients with TASC A lesions, and 85% had either TASC C or D lesions.
Restenosis rates for EI showed that there was an overall tendency for restenosis to increase as the severity of the lesion increased, with TASC D lesions showing the highest restenosis rates. On univariate analysis, there was no statistical difference according to TASC classification, but multivariate analysis showed that TASC D was a significant risk factor for increased restenosis. DM and male gender were also significant risk factors for EI on both univariate and multivariate analyses. The increased restenosis rates for EI in TASC D lesions demonstrate that the severer the lesion, the higher the risk of restenosis. However, this does not prove that EI should not be considered as first-line treatment for TASC D lesions unless we can demonstrate that BS is significantly better than EI. Therefore, EI and BS were compared for the relatively more severe TASC C and D lesions to verify the guidelines suggested by the TASC II Working Group. Our results showed that for TASC C and D lesions, BS had a tendency for better patency rates compared to EI in the long-term, but this difference was not statistically significant. A longer follow-up period might change these results, widening the difference significantly between EI and BS. But for the moment, our results suggest that from the anatomical point of view only, EI is a good treatment option for TASC C and D lesions, and can be considered as a first-line choice.
As mentioned above, anatomical improvement does not always correlate with functional improvement, so the next step was to compare the functional outcomes for the same TASC C and D lesion patients. Both EI and BS showed an improved functional outcome after treatment, but in order to know which treatment modality was better in improving functional ability, the differences in scores were analyzed. The SF-36 (PH only) showed a significant difference in favor of BS, but in the case of the WIQ, although the difference was higher for BS (0.307±0.241 vs. 0.193±0.229), it failed to show statistical significance. However, it is important to notice that the WIQ only measures the walking ability of the patient, while the SF-36 (PH only) measures the overall functional ability, including factors such as general health or bodily pain, and therefore the SF-36 (PH only) is better in assessing overall functional improvement than the WIQ. From these results we can suggest that although anatomically EI and BS showed no difference in TASC C and D lesions, BS had a better overall functional outcome. Therefore in terms of functional improvement, BS can be considered as first-line treatment for TASC C and D lesions.
Recent advances in medicine have brought about a paradigm shift from a doctor-oriented approach to a patientoriented approach in the treatment of diseases. Traditionally, results of clinical studies such as radiologic studies or laboratory tests were the most important factors when diagnosing and treating a disease. These factors are of course important, but nowadays there is a trend for medical treatment to require something more than this. Increased medical knowledge of the patients and an increased desire for better health have changed therapeutic approaches in many diseases. This is the main reason we considered functional outcomes in our study. From our clinical experience, we have found that anatomic patency does not always correlate with functional outcome. Some patients feel no symptoms even with a significantly higher degree of arterial stenosis, while other patients feel much more pain with a lower degree of stenosis. Therefore, we aimed at investigating the functional outcome to see how patients actually felt after treatment, not simply relying on angiographic results to determine treatment success. Our results show that statistically there is no significant difference in restenosis rates for EI in all TASC lesions. This means that theoretically, EI could be used for all lesions as first-line treatment. Furthermore, patency rates between EI and BS showed no significant difference in TASC C and D lesions which again support the theory that anatomically EI could be used for all TASC lesions. However, our studies of functional outcome have demonstrated that BS has better patient outcome than EI for TASC C and D lesions, therefore BS should be considered first in the treatment of TASC C and D lesions, and EI should be considered if the patient is a high risk surgical candidate.
Recent studies have shown the increasing role of EI in the treatment of PAOD, with extension of the indication for EI to all TASC categories, contrary to the TASC II guidelines. The BASIL Trial(7) suggested that both EI and BS had similar amputation-free survival and that BS, in the short term, was more expensive in terms of cost. Kudo et al.(9) reported that EI could be used as first-line procedure whenever possible, and not limited to patients who cannot undergo BS. Dippel et al.(17) suggested that EI in TASC D lesions for claudication was safe and effective in the improvement in quality of life without increasing the risk of amputation. Our results also suggest that, in the anatomical point of view, EI could be applied to all patients irrespective of TASC classification and initial symptom presentation. However, none of the above mentioned studies managed to verify the functional status of the patients. Our study is one of the few studies that considered functional outcome as well as anatomical outcome. Taylor et al.(18) reported that functional outcome was not significantly affected by the type of treatment (EI or BS) or by the level of disease treated (aortoiliac, infrainguinal, or both). However, our results showed that functional outcome was better for BS than EI.
Our 1-year and 2-year restenosis rates for EI were 20.1% and 41.1% respectively, which were comparable to other studies reported previously.(19,20) This proves that our EI results were up to the standard of other major institutions. However our study has several limitations. The retrospective nature and the short follow-up period were limitations. As previously mentioned, a longer study period might have changed the results, especially for the comparison between EI and BS in the anatomical aspect. A referral bias might have affected the results, since the study was performed in a single institution, and the fact that the survey was performed by telephone on a retrospective basis might have caused a recall bias. Finally the sample size was not large enough.
In conclusion, EI for the management of PAOD showed almost equivalent patency rates to those of BS for all range of lesions and irrespective of initial symptom presentation. However, for TASC C and D lesions, BS is still a viable treatment modality on the basis of improved functional outcomes.
Figures and Tables
Fig. 2
Restenosis rates for endovascular intervention according to Trans Atlantic Inter-Society Consensus (TASC) II classification.

Fig. 3
Patency rates between endovascular intervention (EI) and bypass surgery (BS) for Trans Atlantic Inter-Society Consensus (TASC) C and D lesions.
ACKNOWLEDGEMENTS
We thank Minjung Woo, Physician Assistant and Hanmi Yun, Registered Vascular Technician for their contributions in data collection and analysis.
References
1. Norgren L, Hiatt WR, Dormandy JA, Nehler MR, Harris KA, Fowkes FGR. Inter-Society Consensus for the management of peripheral arterial disease (TASC II). J Vasc Surg. 2007. 43:S5–S67.
2. Hirsch AT, Criqui MH, Treat-Jacobson D, Regensteiner JG, Creager MA, Olin JW, et al. Peripheral arterial disease detection, awareness, and treatment in primary care. JAMA. 2001. 286:1317–1324.
3. Hunink MG, Wong JB, Donaldson MC, Meyerovitz MF, de Vries J, Harrington DP. Revascularization for femoropopliteal disease. A decision and cost-effectiveness analysis. JAMA. 1995. 274:165–171.
4. Albers M, Romiti M, Brochado-Neto FC, Pereira CA. Meta-analysis of alternate autologous vein bypass grafts to infrapopliteal arteries. J Vasc Surg. 2005. 42:449–455.
5. van der Zaag ES, Legemate DA, Prins MH, Reekers JA, Jacobs MJ. Angioplasty or bypass for superficial femoral artery disease? A randomised controlled trial. Eur J Vasc Endovasc Surg. 2004. 28:132–137.
6. Hobbs SD, Yapanis M, Burns PJ, Wilmink AB, Bradbury AW, Adam DJ. Peri-operative myocardial injury in patients undergoing surgery for critical limb ischaemia. Eur J Vasc Endovasc Surg. 2005. 29:301–304.
7. Adam DJ, Beard JD, Cleveland T, Bell J, Bradbury AW, Forbes JF, et al. Bypass versus angioplasty in severe ischaemia of the leg (BASIL): multicentre, randomised controlled trial. Lancet. 2005. 366:1925–1934.
8. Haider SN, Kavanagh EG, Forlee M, Colgan MP, Madhavan P, Moore DJ, et al. Two-year outcome with preferential use of infrainguinal angioplasty for critical ischemia. J Vasc Surg. 2006. 43:504–512.
9. Kudo T, Chandra FA, Ahn SS. The effectiveness of percutaneous transluminal angioplasty for the treatment of critical limb ischemia: a 10-year experience. J Vasc Surg. 2005. 41:423–435.
10. Molloy KJ, Nasim A, London NJ, Naylor AR, Bell PR, Fishwick G, et al. Percutaneous transluminal angioplasty in the treatment of critical limb ischemia. J Endovasc Ther. 2003. 10:298–303.
11. Nasr MK, McCarthy RJ, Hardman J, Chalmers A, Horrocks M. The increasing role of percutaneous transluminal angioplasty in the primary management of critical limb ischaemia. Eur J Vasc Endovasc Surg. 2002. 23:398–403.
12. Ware JE, Snow KK, Kosinski M, Gandek B. SF-36 Health Survey: Manual and Interpretation Guide. 1993. Boston: New England Medical Center, Health Institute.
13. Regensteiner JG, Steiner JF, Panzer RJ, Hiatt WR. Evaluation of walking impairment by questionnaire in patients with peripheral arterial disease. J Vasc Med Biol. 1990. 2:142–152.
14. McDermott MM, Mehta S, Liu K, Guralnik JM, Martin GJ, Criqui MH, et al. Leg symptoms, the ankle-brachial index, and walking ability in patients with peripheral arterial disease. J Gen Intern Med. 1999. 14:173–181.
15. Rutherford RB, Baker JD, Ernst C, Johnston KW, Porter JM, Ahn S, et al. Recommended standards for reports dealing with lower extremity ischemia: revised version. J Vasc Surg. 1997. 26:517–538.
16. Ahn SS, Rutherford RB, Becker GJ, Comerota AJ, Johnston KW, McClean GK, et al. Society for Vascular Surgery. International Society for Cardiovascular Surgery. Reporting standards for lower extremity arterial endovascular procedures. J Vasc Surg. 1993. 17:1103–1107.
17. Dippel E, Shammas N, Takes V, Coyne L, Lemke J. Twelve-month results of percutaneous endovascular reconstruction for chronically occluded superficial femoral arteries: a quality-of-life assessment. J Invasive Cardiol. 2006. 18:316–321.
18. Taylor SM, Kalbaugh CA, Blackhurst DW, Cass AL, Trent EA, Langan EM 3rd, et al. Determinants of functional outcome after revascularization for critical limb ischemia: an analysis of 1000 consecutive vascular interventions. J Vasc Surg. 2006. 44:747–755.
19. Black JH 3rd, LaMuraglia GM, Kwolek CJ, Brewster DC, Watkins MT, Cambria RP. Contemporary results of angioplasty-based infrainguinal percutaneous interventions. J Vasc Surg. 2005. 42:932–939.
20. Surowiec SM, Davies MG, Eberly SW, Rhodes JM, Illig KA, Shortell CK, et al. Percutaneous angioplasty and stenting of the superficial femoral artery. J Vasc Surg. 2005. 41:269–278.




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download