Abstract
Purpose
This study evaluated the usefulness of a new scoring system in diagnosing acute appendicitis which expresses the patient's symptoms, physical examination, and laboratory findings more clearly and objectively.
Methods
A prospective study was conducted with 314 patients who were hospitalized with suspicion of acute appendicitis. After analyzing the symptoms, physical examination, and laboratory findings, 10 meaningful variables were selected, each of which were scored separately. The diagnostic value of the new scoring system was evaluated, and analyzed in comparison to the preexisting Alvarado score.
Results
Ten variables including vomiting, migration pain, fever, Dunphy's sign, Rovsing's sign, tenderness, rebound tenderness, increased white blood cell counts, increased neutrophil proportion, and increased CRP levels were associated with acute appendicitis. The new scoring system is developed by applying 1 point for each variable, with a total score of 10 points. In the new scoring system, a score above 5 points had sensitivity of 0.75, specificity of 0.73, positive predictive value of 0.92, and diagnostic accuracy of 0.71. The area under the receiver operating characteristic curve was 0.80, which is larger than 0.72 of the preexisting Alvarado score, and thus has a higher diagnostic accuracy. As acute appendicitis progresses, the average score tends to become significantly higher (P=0.001).
Conclusion
The new scoring system, which objectively reflects the clinical variables of the patient's symptoms, physical examination and laboratory findings, will be useful in accurately diagnosing acute appendicitis and in quickly deciding a therapeutic policy in patients with right lower abdominal pain.
Acute appendicitis is the most common abdominal emergency demanding an imperative operation, although it can be treated without complication with early diagnosis and operation. Presently, there is no perfectively accurate diagnostic examination tool if the symptom is ambiguous, the diagnostic process takes longer and the operation is delayed, resulted in increasing the possibility of complications. On the other hand, any hasty operation without accurate diagnosis will typically lead to a negative appendectomy, resulting in increase morbidity and costs.(1-4)
Diagnostic approaches include symptoms, physical examination, laboratory findings and imaging tools such as abdominal ultrasonic and CT examinations. Unfortunately, the accuracy of ultrasonic examination depends on the operators' proficiency, and it is not available at night usually in my hospital.(5) The abdominal CT examination assumes a risk of radiation exposure and let alone rising cost when used recklessly.(6) Although acute appendicitis can be diagnosed with clinical variables such as symptoms, physical examination and simple laboratory findings, the majority of surgeons tend to rely on abdominal ultrasonic or CT examination for a more objective diagnosis. Not only in clinically atypical acute appendicitis but also in typical ones, probable diagnosis or treatment differs depending on the doctors' propensity. This tendency is getting more common as resolving appendicitis without treatment is known in equivocal signs of appendicitis.(7,8) Accordingly, several diagnostic scoring systems for objective diagnosis of acute appendicitis have been introduced. Among those systems, the Alvarado scoring system released in 1986 by Alvarado et al.(9) is reported to be relatively simple to apply and guarantee high efficacy. As a rule, the Alvarado scoring system is used to determine diagnostic values of appendicitis with abdominal ultrasonic or CT examination. As an approach to reduce the negative appendectomy accounting for over 30% in the 1980s, the Alvarado score refers to a scoring system for appendicitis diagnosis using 8 variables such as anorexia, nausea/vomiting, migration of pain to the right iliac fossa (RIF), low-grade fever, tenderness, rebound tenderness, leukocytosis and neutrophil proportion increase with a total of 10 points. The Alvarado scoring system is made from retrospective study and the resulting scores can vary depending on patients' subjective elements and doctors' proficiency. Further, in the Alvarado scoring system, whether each variable is statistically and independently relevant to acute appendicitis and valid as an inflammatory reaction variable are not sufficiently accounted for. As such, this study adopted general symptoms, physical examination findings and laboratory findings that are commonly known to be associated with acute appendicitis and took a prospective approach to find out whether each of such variables are independently related to acute appendicitis and valid as an inflammatory reaction variable. Moreover, we tried to modify the system for more objective application of several elements in the Alvarado score, which is prone to subjective judgment, and investigate its feasibility and diagnostic value.
Between October 2008 and June 2009, 314 patients were selected as study subjects in 4 general hospitals located in Cheongju City, Chungcheongbuk-do. Those patients were hospitalized with RLQ pain and suspected appendicitis. Study subjects consisted of 157 males (50%) and 157 females (50%).
A prospective study was conducted with such variables as the elapsed time from the onset of symptoms to arrival at hospitals, symptoms, physical examination and laboratory findings. The final diagnosis was made from result of the histopathologic finding on tissues excised in operation. For a statistical analysis, SPSS version 12.0 (SPSS Inc., Chicago, IL, USA) was used to apply t-test and Chi-square test to the variables, and P-values less than 0.05 were determined to be statistically significant. A 'new scoring system' was developed by adopting independent variables found significant and then assigning a point to each variable. B-score gained with new scoring system was compared with A-score estimated with the Alvarado scoring system in terms of sensitivity, specificity, positive predictive value, negative predictive value, accuracy and receiver operating characteristic (ROC) curve. Also, any relevance to inflammation progress was analyzed. Our protocol was approved by the Chungbuk National University Hospital institutional review board.
Among 314 patients hospitalized with suspected acute appendicitis, 274 patients (87.3%) were operated, while 40 patients (12.7%) were treated with conservative managements to observe the progress. Twenty-four patients (8.7%) out of those 274 patients who received operation were negative appendectomy. The histopathologic finding found acute appendicitis in 250 patients (79.6%), among whom 133 were male (53.2%) and 117 were female (46.8%), and whose average age was 32.8 years (male: 31.0 years, female: 34.9 years), which was slightly older than those in other reports. Among 40 patients who received conservative treatments, 16 were found to have acute gastroenteritis, 12 diverticulitis, 6 mesenteric lymphadenitis, and 6 pelvic inflammatory disease (PID). Among 24 patients who underwent negative appendectomy, 2 patients were determined to have mucocele, 13 acute gastroenteritis, 3 diverticulitis, 4 mesenteric lymphadenitis, and 2 PID.
Then, each pre-surveyed variable was investigated for any relevance to appendicitis, followed by analyses on its significance (Table 1).
Age was found to have nothing to do with appendicitis (P=0.08). The most number of patients were in their teens and thirties, and those over 60s accounted for more than 10%. The elapsed time from the onset of symptoms to arrival at hospitals in appendicitis patients was 32 hours on average, and 36 hours in non-appendicitis patients, which showed no significant difference between two groups (P=0.3). As for gender differences, males were found to have relevance to appendicitis (P=0.02). While females were considered to have relevance to female diseases like PID. So, gender was excluded from further analyses as it was not a measure indicating inflammatory factors.
Anorexia was assessed not to have relevance to appendicitis (P=0.28), and was excluded from further analyses. The nausea/vomiting on the Alvarado score was put together as the vomiting variable, which was found to appear at the initial stage of inflammatory factors and be closely associated with appendicitis (P=0.01). The migration of pain from the epigastric or the periumbilical area to the right lower quadrant was also found to be relevant to appendicitis (P=0.001).
Body temperature was found to have relevance to appendicitis (P=0.02). In the present study, fever of 38℃ or higher was set as a variable included in further analyses. Both Dunphy's sign where patients feel pain upon coughing and tenderness upon percussion were found relevant to appendicitis (P=0.001). As the two physical examinations share lots of similar mechanisms, they were combined into the Dunphy's sign, which was included in further analyses. Rovsing's sign used to identify indirect tenderness was also relevant to appendicitis (P=0.01). As tenderness and rebound tenderness showed close relevance to appendicitis, both were included in further analyses (P=0.003, 0.001).
White blood cell count was closely related to appendicitis (P=0.002), so the present study adopted 10,000/mm3 or more as a variable. Neutrophil proportion increase was included as a significant variable when it was more than 75% (P=0.001), and CRP concentration rise was employed as a significant variable at 10 mg/L plus (P=0.001).
Variables adopted to get the B-score included vomiting and migration of pain as patients' symptoms; fever (body temperature ≥38℃), Dunphy's sign, Rovsing's sign, tenderness and rebound tenderness as physical examination; and white blood cell count of 10,000/mm3 or more, neutrophil proportion of more than 75% and CRP concentration of higher than 10 mg/L as laboratory finding values. Then, each variable was assigned 1 point, adding up to the total of 10 points for the 'new scoring system' (Table 2). The score gained from each patient based on new scoring system was named B-score, which was, in turn, compared with the A-score estimated with the Alvarado scoring system. The A-score in acute appendicitis patients was 6.4 (±2.0) points, while 4.7 (±1.9) in non-appendicitis patients, indicating a significant difference (P=0.001). The B-score in acute appendicitis patients was 5.9 (±2.1) points, while 3.6 (±1.7) in non-appendicitis ones, indicating a significant difference as well (P=0.001).
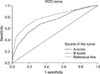
The area under the ROC curve in A-score was 0.72, while 0.80 in B-score, indicating a high differentiation between the two (Fig. 1). When ROC curve, sensitivity, specificity, positive predictive value, negative predictive value and accuracy were summed up, the A-score cut-off values were in order of 6 and 7 points, and those of the B-score were 5 and 6 points. Thus, 1-point difference was found in the cut-off value between A- and B-score. It was found here that when the A-score was higher than 7 points, sensitivity was 0.53, specificity 0.81, positive predictive value 0.92, and diagnostic accuracy 0.59. Also, when the A-score was more than 6 points, sensitivity was 0.68, specificity 0.67, positive predictive value 0.89 and diagnostic accuracy 0.68. Meanwhile, when the B-score was higher than 6 points, it was found that sensitivity was 0.61, specificity 0.86, positive predictive value 0.94, and accuracy 0.66. Also, when the B-score was over 5 points, sensitivity was 0.75, specificity 0.73, positive predictive value 0.92 and accuracy 0.71 (Table 3). When the B-score cut-off value, of 5 points, was compared with the A-score cut-off value of 6 points, sensitivity, specificity, positive predictive value and accuracy were found higher overall.
After operation, the acute appendicitis patients were divided depending on histopathological results, which led to a significant increase in the average of B-score (P=0.001) (Table 4).
Acute appendicitis is a common acute abdominal pain that surgeons frequently encounter. Basically and compared with other diseases, clinical aspects are important in acute appendicitis, in that more than 70% of acute appendicitis is possibly diagnosed based on patients' symptoms, physical examination and laboratory findings. However, atypical clinical symptoms of acute appendicitis account for 30 to 50%.(9,10)
As a diagnostic approach to acute appendicitis, Teicher et al.(11) and Alvarado et al.(9) reported a scoring system in 1983 and 1986, respectively. Since then, a number of reports evaluating its usefulness and feasibility have proved the evaluated accuracy ranges from 76% to 92%.(12,13) Afterward, imaging examinations such as abdominal ultrasonic and CT examinations have proved useful and feasible. To meet the demands of patients or families for accurate diagnoses, abdominal ultrasonic and CT examinations are used more and more. In the present study, the abdominal ultrasonic examination showed sensitivity of 0.95, specificity of 0.72, and accuracy of 0.90. Unfortunately, the abdominal ultrasonic examination has short-comings in that the results differ depending on doctors' proficiency, and that the appendix cannot be observed in case patients are obese or have much intestinal gas, as well as that emergency application is limited. The abdominal CT examination implies a risk of radiation exposure and the contrast media can cause side effects. Further, equivocal appendicitis is highly likely to result in an uncertain diagnosis in abdominal CT examination.(10,14) In this study, abdominal CT examination was found to have sensitivity of 0.93, specificity of 0.87 and accuracy of 0.92.
Through simple history taking and examination, the diagnosis scoring system is conducive to determine whether to conduct an immediate operation or to take additional examinations after further observation on emergency patients or outpatients with suspected acute appendicitis. Also, the system is good for doctors to objectively communicate on different interpretations over examination results. Alvarado score is the best known diagnosis scoring system, but more clear-cut objective variables are required because the process of adopting inflammatory variables is uncertain and subjective variables are included.
In the present study, 10 variables were found independently associated with acute appendicitis. The 10 variables are two symptom variables (migration of pain to the RIF and vomiting); five physical examination variables (fever, Dunphy's sign, Rovsing's sign, tenderness, and rebound tenderness); and three laboratory finding variables (increase in white blood cell, neutrophil proportion and CRP concentration). Thus, each variable is assigned 1 point, adding up to 10 points in total, to get a 'new scoring system.' Especially, Rovsing's sign, CRP concentration, neutrophil proportion and Dunphy's sign were more relevant variables. This indicates that not only laboratory findings but also physical signs are sufficiently worthy inflammatory factors. Gender difference was also found, which may be attributable to diseases seen only in female like PID, but gender was excluded from the scoring system as it was not a suitable inflammatory factor. The B-score gained from this scoring system was found feasible as a diagnostic examination in that the area under the ROC curve was 0.80. When the B-score is more than 5 points, its diagnostic value was determined with the negative appendectomy being less than 10% and with sensitivity and specificity being more than 70%. Particularly, when the score goes over 6, the specificity and the positive predictive value rise to 86% and 94%, respectively, indicating that it is good to conduct an operation. If operation were performed in more than 6 points, 8 patients would undergo negative appendectomy. Actually, 4 patients underwent operation and three of them were diagnosed in abdominal ultrasonic and CT examinations as having appendicitis and found to have diverticulitis and severe colitis. One patient underwent operation without other imaging studies, and was suspected to have an inflammatory appendicitis in operative findings, but determined as being normal in histopathological examination. The remaining 4 patients were found to be normal in abdominal ultrasonic and CT examinations, and observed and determined to have mesenteric lymphadenitis and atypical colitis.
In the original Alvarado scoring system, the nausea/vomiting item was not a significant differential diagnostic variable (P=0.2)(9) but adopted in the diagnosis scoring system. Tenderness is seen in most of the similar diseases as well as appendicitis but adopted and assigned 2 points due to its high sensitivity. The scores for appendicitis and non-appendicitis were found to be 7.71 and 5.24 points, respectively, where more than 6 or 7 points were proposed as appropriate findings for appendicitis. Since then, most studies have set 7 points and plus as a baseline, reporting sensitivity of 0.63~0.87 and specificity of 0.60~0.80.(15,16) The present study also found the sensitivity to be 0.68 and the specificity 0.67 when the score was more than 6 points, and they were 0.53 and 0.81, respectively when the score was more than 7, which showed no difference from other reports.
Existing Alvarado scoring system is not clear in adopting independent variables and contains subjective variables such as anorexia, nausea etc. These subjective variables were found insignificant in this study. Also, tenderness and leukocytosis items were not remarkably significant enough to be given weighted points compared to other variables. The scoring system adopted in this study modified the original system by employing more clear-cut objective variables such as vomiting, Dunphy's sign, Rovsing's sign and CRP and did not impose weighted points lest big differences should appear because of one variable. Vomiting, Dunphy's sign, Rovsing's sign and CRP are reported to be significant independent variables in other studies.(17-19) Recently, Andersson and Andersson(18) reported that vomiting, tenderness, rebound tenderness, body temperature, neutrophil proportion, white blood cell count and CRP concentration are adopted, which supports the approach taken in the present study.
New scoring system is based on simple symptoms, physical examinations and laboratory findings and assigns 1 point to each variable. All in all, the new system yielded a total score less 1 point than that of the original Alvarado system, which probably resulted from adopting variables found to have significant relevance to acute appendicitis. This new system is to be extensively used by raising or lowering the baseline in accordance with doctor's individual examination approaches or propensity. If the score is more than 5 points, diagnosis is possible in more than 70% of patients. On top of anything else, advanced appendicitis leads to sensitivity of more than 90%, adding much more to new scoring system's diagnostic accuracy.
In conclusion, Based on the findings discussed above, this study is to suggest new scoring system as an alternative to diagnose acute appendicitis in patients with abdominal pain in the right lower quadrant. This new system reflects patient's symptoms, physical examination and laboratory findings as objective clinical variables.
If the score is more than 5 points, appendicitis is possibly diagnosed and negative appendectomy can be reduced to less than 10% (when the score is more than 6 points, it is below 5%). New scoring system will be conducive to accurate diagnosis of acute appendicitis in patients with abdominal pain in the right lower quadrant and a swift decision making of treatment strategy.
Figures and Tables
Fig. 1
Comparison of receiver operating characteristic (ROC) curves of Alvarado score (A-score) and new scoring system (B-score). Area under curve of B-score is larger than that of A-score.
References
1. Jones PF. Suspected acute appendicitis: trends in management over 30 years. Br J Surg. 2001. 88:1570–1577.
2. Andersson R, Hugander A, Thulin A, Nyström PO, Olaison G. Indications for operation in suspected appendicitis and incidence of perforation. BMJ. 1994. 308:107–110.
3. Addiss DG, Shaffer N, Fowler BS, Tauxe RV. The epidemiology of appendicitis and appendectomy in the United States. Am J Epidemiol. 1990. 132:910–925.
4. Lewis FR, Holcroft JW, Boey J, Dunphy E. Appendicitis. A critical review of diagnosis and treatment in 1,000 cases. Arch Surg. 1975. 110:677–684.
5. Gupta H, Dupuy DE. Advances in imaging of the acute abdomen. Surg Clin North Am. 1997. 77:1245–1263.
6. Terasawa T, Blackmore CC, Bent S, Kohlwes RJ. Systematic review: computed tomography and ultrasonography to detect acute appendicitis in adults and adolescents. Ann Intern Med. 2004. 141:537–546.
7. Heller MB, Skolnick ML. Ultrasound documentation of spontaneously resolving appendicitis. Am J Emerg Med. 1993. 11:51–53.
8. Andersson RE. Resolving appendicitis is common: further evidence. Ann Surg. 2008. 247:553.
9. Alvarado A. A practical score for the early diagnosis of acute appendicitis. Ann Emerg Med. 1986. 15:557–564.
10. Andersson RE, Hugander A, Ravn H, Offenbartl K, Ghazi SH, Nyström PO, et al. Repeated clinical and laboratory examinations in patients with an equivocal diagnosis of appendicitis. World J Surg. 2000. 24:479–485.
11. Teicher I, Landa B, Cohen M, Kabnick LS, Wise L. Scoring system to aid in diagnoses of appendicitis. Ann Surg. 1983. 198:753–759.
12. Owen TD, Williams H, Stiff G, Jenkinson LR, Rees BI. Evaluation of the Alvarado score in acute appendicitis. J R Soc Med. 1992. 85:87–88.
13. Sun JS, Noh HW, Min YG, Lee JH, Kim JK, Park KJ, et al. Receiver operating characteristic analysis of the diagnostic performance of a computed tomographic examination and the Alvarado score for diagnosing acute appendicitis: emphasis on age and sex of the patients. J Comput Assist Tomogr. 2008. 32:386–391.
14. Perez J, Barone JE, Wilbanks TO, Jorgensson D, Corvo PR. Liberal use of computed tomography scanning does not improve diagnostic accuracy in appendicitis. Am J Surg. 2003. 185:194–197.
15. Chan MY, Teo BS, Ng BL. The Alvarado score and acute appendicitis. Ann Acad Med Singapore. 2001. 30:510–512.
16. Subotić AM, Sijacki AD, Dugalić VD, Antić AA, Vuković GM, Vukojević VS, et al. Evaluation of the Alvarado score in the diagnosis of acute appendicitis. Acta Chir Iugosl. 2008. 55:55–61.
17. Jahn H, Mathiesen FK, Neckelmann K, Hovendal CP, Bellstrøm T, Gottrup F. Comparison of clinical judgment and diagnostic ultrasonography in the diagnosis of acute appendicitis: experience with a score-aided diagnosis. Eur J Surg. 1997. 163:433–443.
18. Andersson M, Andersson RE. The appendicitis inflammatory response score: a tool for the diagnosis of acute appendicitis that outperforms the Alvarado score. World J Surg. 2008. 32:1843–1849.
19. Wu HP, Huang CY, Chang YJ, Chou CC, Lin CY. Use of changes over time in serum inflammatory parameters in patients with equivocal appendicitis. Surgery. 2006. 139:789–796.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download