INTRODUCTION
There is general consensus that the anatomical extent of gastric cancer is an independent prognostic factor. This has been shown for depth of tumor invasion, involvement of regional lymph nodes and presence of distant metastasis (TNM). Prognostic factors in cancer serve to predict clinical outcome for individual patients and are particularly useful in identification of subgroups at high risk of relapse. TNM and pTNM describe the anatomical extent of cancer in general without considering treatment.(1)
A curative tumor resection must still be recognized as the most powerful prognostic variable among treatment-related factors, and in addition, there is consensus that the quality of the resection is relevant to survival.(2) The only proven, potentially curative treatment for gastric cancer is surgical resection of all gross and microscopic disease. The R classification system indicates the amount of residual disease left after tumor resection.(3) R0 indicates no gross or microscopic residual disease, R1 indicates microscopic residual disease, and R2 signifies gross residual disease. R0 is appropriate for cases in which residual tumor cannot be detected by currently available diagnostic modalities. R0 classification does not exclude nondetectable residual tumor, which may give rise to tumor recurrence or metastasis during follow-up. R0, in fact, corresponds to no detectable residual tumor and may not be identical to cure.(4)
Therefore, even after what is felt to be a "curative" R0 gastrectomy, disease recurs in both regional and/or distant sites. Rationally, patients with early stage gastric cancers have a good to excellent chance of cure with surgery alone. However, patients with more advanced stages, even if all visible disease has been resected with negative microscopical margins, have a far worse outcome. The risk of recurrence after resection increases as stage increases. The high risk for recurrence with surgery alone has led to extensive investigation of the use of postoperative adjuvant, and more recently, perioperative systemic therapy.
According to the Japanese Classification of Gastric Carcinoma, the curative potential of gastric resection is classified as Resection A, B, and C. Resection A surgery means no residual disease with high probability of cure and implies resections satisfying all of the following conditions: T1 or T2; N0 treated by D1, 2, 3 resection or N1 treated by D2, 3 resection; M0, P0, H0, CY0 and proximal and distal margins >10 mm.(5) However, some patients die of recurrent disease even after Resection A surgery.
Therefore, we evaluated the clinical implication of Resection A surgery to identify whether quality of surgery can be used as a selection factor for adjuvant therapy in patients with gastric cancer.
METHODS
During a 10-year period from 1990 to 1999, 902 patients with gastric cancer underwent Resection A surgery at the Department of Surgery, Kyungpook National University Hospital (Table 1). Their median age was 57 years old, ranging from 26 to 83.
Depending on location and macroscopic type of gastric cancer either total or distal subtotal gastrectomy was selected. Extent of lymph node dissection was selected at the discretion of a surgeon according to his clinical judgment regarding the extent of disease. Roux-en-Y reconstruction with a stapled esophagojejunostomy was used after total gastrectomy. Billroth I gastroduodenostomy or Billroth-II gastrojejunostomy was used after distal subtotal gastrectomy.
The resected specimen was examined according to the Japanese Classification of Gastric Carcinoma. TNM category and stage were assigned using criteria provided by the sixth edition of the International Union Against Cancer (UICC) classification.(1)
Postoperative adjuvant chemotherapy after Resection A surgery has not been recommended by the surgeons. However, 5-fluorouracil and cisplatin were administered postoperatively in some cases at the patients' request.
The proportions of patients with a given characteristic were compared by the chi-square test. Survival for all discharged patients was calculated from the date of operation until death or last date of follow-up, and Kaplan-Meier survival curves were plotted and compared by the log-rank test. A multivariate analysis was done by the Cox proportional hazards model. The differences were judged to be significant with a P-value of <0.05.
RESULTS
Twenty-nine patients were lost to follow-up (follow-up rate, 96.8%). Among all discharged patients, 77 patients (8.5%) died of recurrent disease, 55 patients (6.1%) died without recurrent disease. Five-year survival rate of all discharged patients was 91.6% and 10-year survival rate 87.1%.
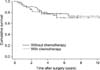
Results of univariate analyses were summarized in Table 2. Statistically significant prognostic factors were depth of invasion (P<0.001), lymph node metastasis (P<0.001), stage (P<0.001), tumor location (P=0.036) and size (P=0.001), extent of gastric resection (P<0.001), and chemotherapy (P<0.001) on univariate analyses.
However, depth of invasion (P=0.001), lymph node metastasis (P<0.001), and total gastrectomy (P<0.001) emerged as the statistically significant prognostic factors on a multivariate analysis (Table 3).
DISCUSSION
The prognosis for patients with gastric cancer is, to a large extent, dependent on the extent of disease at the time of diagnosis.(6) Our results also showed that the depth of tumor invasion and lymph node metastasis were strong prognostic indicators even after Resection A surgery.
A curative tumor resection must still be recognized as the most powerful prognostic variable of treatment-related factors. The optimal surgical management of gastric cancer must be tailored to the extent and location of disease. In the absence of distant metastatic spread, an aggressive surgical procedure to achieve macroscopically and microscopically complete surgical resection of tumor is justified. There is consensus that the quality of the resection is relevant to survival. Allgayer and colleagues reported that the hospital was an independent prognostic factor with a higher probability of survival for patients operated in centers with a broad experience in oncological surgery.(2)
Even after what is felt to be a curative gastrectomy, disease recurs in both regional and/or distant sites in the majority of patients with stage II or III gastric cancers. Efforts to improve these poor results have focused on developing effective pre- and postoperative systemic and regional adjuvant therapies. There are a few reports on the effectiveness of adjuvant chemotherapy for gastric cancer.(7-9) It is important to identify patients with apparent early-stage disease who will not be cured by surgery alone and, conversely, patients with late-stage cancer who will not have residual disease after surgery and in whom additional therapy is not needed.(6) Additionally, the lower-risk patients should be spared the risks for toxicity associated with adjuvant chemotherapy.
Resection A surgery encompasses both anatomical and therapeutic components. Depth of invasion should be T1 or T2 and there is no distant metastasis. Therapeutic components are resection margins and extent of lymph node dissection. Stage IA (T1N0M0) and IB (T2N0M0) fulfill the anatomic components of Resection A surgery. These diseases fulfill the therapeutic components even with D1 dissection when proximal and distal resection margins are free of disease. When a patient has T1N1M0 (stage IB) or T2N1M0 (stage II) disease, Resection A surgery requires D2 dissection to satisfy its therapeutic components.
The role of D2 lymphadenectomy in the surgical treatment of gastric cancer remains controversial. The first evidence of a survival benefit for a D2 dissection was in 1981 by Kodama and colleagues.(10) Multiple other Japanese studies have confirmed these findings. However, randomized controlled trials in the West of D2 versus D1 dissections for gastric cancer have failed to demonstrate a survival benefit for D2 dissection.(11,12) Several studies have demonstrated that D2 lymph node dissection, performed without increased risk of morbidity and mortality, is associated with better long-term survival. The phase II trial conducted by the Italian Gastric Cancer Study Group reported a survival benefit of pancreas-preserving D2 lymphadenectomy when performed in experienced cancer centers.(13) The studies from Austria(14) and Spain(15) also showed an improved survival in patients with resected gastric cancer.
National Comprehensive Cancer Network (NCCN) Clinical Practice Guidelines in Oncology™(16) as well as gastric cancer treatment guidelines in Japan(17) recommends stage-oriented therapeutic strategy. At present, patients with stage I gastric cancers have a good to excellent prognosis, and cure rates can exceed 80% with surgery alone.(6) However, NCCN guidelines recommend perioperative chemoradiation therapy or chemotherapy not only in stage II (T2N1M0) but also in stage I (T2N0M0). The Japanese guidelines recommend adjuvant chemotherapy in stage II.
Clinical stage of the gastric cancer at the time of diagnosis is crucial factor in selecting initial treatment modality. However, the preoperative identification of patients with lower-risk disease (for whom surgery alone may be adequate) and those with higher-risk disease (for whom adjuvant therapy may be beneficial) remains difficult.(6) Gastrectomy with D1 dissection is sufficient in stage IA (T1N0M0) and T2N0M0 of stage IB. However, in T1N1M0 of stage IB, D2 dissection is required for sufficient surgery. Stage II includes T1N2M0, T2N1M0, and T3N0M0. Among them, Resection A surgery can be performed only in T2N1M0. When the surgery is sufficient, adjuvant therapy is not needed. Our results showed that adjuvant chemotherapy did not increase the survival rate after Resection A surgery in patients with T2N1M0 disease. Adjuvant treatment can be considered in patients with T1N2M0 or T3N0M0 disease, because T1N2M0 disease does not fulfill the therapeutic components of the Resection A surgery and T3N0M0 disease does not fulfill the anatomic components. Sakuramoto and colleagues reported that there was statistically significant increase in 3-year survival rate of surgery with adjuvant chemotherapy group as compared to the surgery-only group. About 50% of patients had stage II disease. However, the proportions of T1N2, T2N1, and T3N0 were not defined in this report.(9)
In conclusion, most patients survive without recurrent disease after Resection A surgery for gastric cancer and chemotherapy did not increase survival rate after Resection A surgery. In selecting the patients for adjuvant therapy, both the stage of gastric cancer and the quality of surgery should be considered.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download