Abstract
Purpose
Surgical approaches for papillary thyroid carcinoma remain controversial. Moreover, previous reports regarding surgical strategy for papillary carcinoma of thyroid isthmus are very few. The aims of this study are to analyze the clinicopathologic features of papillary thyroid carcinoma of the isthmus and to develop more appropriate surgical strategies.
Methods
Prospectively, papillary carcinoma arising thyroid isthmus (n=35) was included in this study from June 2006 to December 2008. All of the patients had total thyroidectomy with bilateral central compartment node dissection performed. Lateral nodes were sampled for frozen biopsy when metastasis was suspected by preoperative study. Thirty-five patients, who had unilateral papillary thyroid carcinoma, had total thyroidectomy with bilateral central compartment node dissection as control group and compared with papillary thyroid carcinoma of isthmus.
Results
Lymph node metastasis was higher than control group in patients of isthmus cancer (51% vs 20%, P<0.05). Capsular invasion and multifocality observed in 63% and 23% respectively, but there was no significant difference compared to control group, statistically. Capsular invasion showed a positive correlation with lymph node metastasis by univariate and multivariate analysis. Analysis of ipsilateral nodal metastatic distribution revealed no definite metastatic pattern. Tracheal adhesion was observed in 4 cases of isthmus cancer group.
Figures and Tables
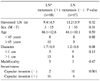
Table 1
Comparison of surgical data between isthmic papillary cancer and non isthmic papillary cancer

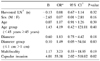
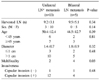
Table 2
Comparison of surgical data between isthmic papillary microcarcinoma and no isthmic papillary microcarcinoma

References
1. Sugenoya A, Shingu K, Kobayashi S, Masuda H, Takahashi S, Shimizu T, et al. Surgical strategies for differentiated carcinoma of the thyroid isthmus. Head Neck. 1993. 15:158–160.
2. Bilimoria KY, Bentrem DJ, Ko CY, Stewart AK, Winchester DP, Talamonti MS, et al. Extent of surgery affects survival for papillary thyroid cancer. Ann Surg. 2007. 246:375–384.
3. Noguchi M, Yamada H, Ohta N, Ishida T, Tajiri K, Fujii H, et al. Regional lymph node metastases in well-differentiated thyroid carcinoma. Int Surg. 1987. 72:100–103.
4. Noguchi M, Kinami S, Kinoshita K, Kitagawa H, Thomas M, Miyazaki I, et al. Risk of bilateral cervical lymph node metastases in papillary thyroid cancer. J Surg Oncol. 1993. 52:155–159.
5. Mirallie E, Visset J, Sagan C, Hamy A, Le Bodic MF, Paineau J. Localization of cervical node metastasis of papillary thyroid carcinoma. World J Surg. 1999. 23:970–974.
6. Shigematsu N, Takami H, Kubo A. Unique treatment policy for well-differentiated thyroid cancer in Japan: results of a questionnaire distributed to members of the Japanese Society of Thyroid Surgery and the International Association of Endocrine Surgeons. Endocr J. 2006. 53:829–839.
7. McConahey WM, Hay ID, Woolner LB, van Heerden JA, Taylor WF. Papillary thyroid cancer treated at the Mayo Clinic, 1946 through 1970: initial manifestations, pathologic findings, therapy, and outcome. Mayo Clin Proc. 1986. 61:978–996.
8. Ortiz S, Rodriguez JM, Soria T, Perez-Flores D, Pinero A, Moreno J, et al. Extrathyroid spread in papillary carcinoma of the thyroid: clinicopathological and prognostic study. Otolaryngol Head Neck Surg. 2001. 124:261–265.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download