Abstract
Purpose
The design of this study was to determine the most influential factor(s) on post-transplant immunological consequences, particularly with regard to the role of killer cell immunoglobulin-like receptors (KIRs) and their ligands (type I human leukocyte antigen (HLA)) in unstable liver function.
Methods
Retrospectively collected data from 319 recipients undergoing adult living donor liver transplantation (LDLT) using a right lobe graft between January 2002 and August 2008 were analyzed. Patients were categorized according to the serum alanine transaminase (ALT) pattern; stable ALT pattern was defined as ALT pattern during 3 months post-transplantation, except for initial 2 weeks post-transplantation, in which 2 times or less additional elevation(s) of serum alanine transaminase (ALT) (≥80 IU/L) were observed. When a serum ALT pattern showed fluctuating and/or unpredictable nature, it was defined as an unstable pattern. In addition, genetic information of KIRs and HLA-C allotypes received from 68 recipients and 59 donors was analyzed by way of polymerase chain reaction using sequence-specific primers (PCR-SSP) to determine the factor(s) influencing a serum ALT pattern.
Results
Among 319 LDLT recipients included in this study, the actual incidences of AR and unstable ALT pattern were 13.4% (43/319) and 42.3% (135/319), respectively. Unstable ALT pattern correlated with poorer survival following LDLT than stable pattern (P<0.000). Genetically, unstable ALT pattern was related to recipients carrying KIR2DL2(+)/KIR2DS2(+) combined with the heterogeneous HLA-C allotype (HLA-C1/C2), (relative risks 45.0, 95% confidence interval 2.160~937.321; P=0.013).
From an immunological standpoint, the transplanted liver represents a continuous source of human leukocyte antigen (HLA) alloantigens capable of inducing a rejection response at any time post-transplantation necessitating life-long immunosuppression. At the same time, unlike in other organ transplantations, i.e., renal transplantation, deliberate efforts to satisfy immunological acceptance are not highly required. Some recipients maintain stable levels of serum liver enzymes with minimal requirement of immunosuppressant regimens. Actually, following orthotopic liver transplantation, successful withdrawals of immunosuppressants were reported in 19% to 42% of patients.(1-4) Concerning living donor liver transplantation (LDLT), Takatsuki et al.(5) reported that 38.1% (24/63) achieved complete withdrawal of tacrolimus with a median drug-free period of 23.5 months. Thus, immunological background, different from other transplantations, might have affected these outcomes. If there exists a certain patient population from which immunosuppressants can be safely withdrawn, further points must be clarified including the characteristics of these patients and the determinant factors. Actually, we did not reach the point of the complete withdrawal in our patients, but we did find certain patients who maintain stable liver enzymes with minimal immunosuppressants.
Aspartate transaminase (AST) and alanine transaminase (ALT) are enzymes associated with liver parenchymal cells. These liver enzymes are released into the blood when the liver is damaged. It is natural to have elevated liver enzymes just after liver transplantation (LT) but having additional or persistent elevation suggests that other medical problems such as acute rejection (AR) and other immunological changes are evoking hepatocyte damage. However, the magnitude of liver enzymes may simply reflect a certain point of the liver condition. They can also fluctuate, but allowances cannot be made for such patterns when we measure the magnitude of serum liver enzymes at a single timepoint. In addition, AR - the only known immunological parameter - can be diagnosed based on the invasive procedure which can not be carried out all the suspected recipients. Therefore, in addition to AR, we introduced the liver enzyme pattern based on the serum ALT changing characteristics during 3 months post-transplantation to assess the immunological function of the liver.
The human immune system can be largely divided into innate and acquired immunity.(6) In transplantation, innate immunity provides rapid recognition and initial defense against the foreign material - an allograft - at the expense of selectivity. Its main components are natural killer (NK) cells. During this process of innate immunity, the allograft also is recognized by host T cells, by direct and/or indirect allorecognition. Later, T cells present a specific attack based on the characteristics of the allograft, of which process is termed as acquired immunity. Killer cell immunoglobulin-like receptors (KIR) play a role in both of these processes.(6-8) KIRs are major receptors of the NK cell mediating innate immunity and are also involved in acquired immunity because certain subsets of T cells express KIRs on their surface.
KIR genes are located on chromosome 19q13.4 and have high diversity (6,7) and accordingly, KIRs, the end products of KIR genes, have distinct polymorphisms. KIRs are mainly located on the surface of NK cells, and certain sets of T cells also express them and T cell receptors (TCR).(9,10) HLA type I antigens (A, B & C) are ligands for KIRs.(11) Among HLA-C alleles (HLA-C1 & HLA-C2), HLA-C1 indicates the HLA-C allele that carries an asparagine at position 80 (with a lysine at position 77) and includes HLA-Cw*01, 03, 07, and 08, while HLA-C2 carries a lysine at position 80 (with an asparagine at position 77) and includes HLA-Cw*02, 04, 05, and 06.(12) Interactions between the KIR and KIR ligand (type I HLA) initiate signals that determine the activity of the NK cells (or T cells) expressing the KIRs. The signals transmitted into the NK cell (or T cell) can be activating or inhibitory, according to the nature of the KIR.
In our study, we investigated whether serum ALT pattern can reflect the immunological consequences including post-transplantation patient survival. And, if the serum ALT pattern were proved to bear clinical significance, we tried to find the most influential factor(s) contributing to its stability taken clinical data and genetic information concerning KIRs and their ligands as well into consideration.
Retrospectively collected data from patients undergoing adult LDLTs using a right lobe graft in the Department of Liver Transplantation, the Catholic University of Korea, between January 2002 and August 2008 were reviewed. Patients who survived less than 3 months were excluded from the study. In addition, patients who had experienced complications originated from surgical (or technical) causes were also excluded. Information on 319 patients was available. The protocol and study design of the present trial were approved and conducted according to the guidelines of the Ethical Committee of the Catholic University of Korea. Patients were categorized according to 2 criteria: AR and serum ALT pattern. In this study, we only considered a case as AR when it was clinically acknowledged and histologically diagnosed according to an internationally accepted consensus document on AR.(13,14) Recipients were also divided according to the sequential ALT pattern during 3 months post-transplantation. Stable ALT pattern indicates an ALT pattern during which period, except for initial 2 weeks post-transplantation, 2 times or less additional elevation(s) of serum ALT (≥80 IU/L) were observed. When a serum ALT pattern showed fluctuating and/or unpredictable nature, it was termed as an unstable pattern.
Clinically, all variable considerations were classified as recipient factors, donor factors or donor-recipient interrelationship factors and analyzed. Recipient factors included recipient's age and sex, underlying liver diseases, preoperative serum ALT level, serum creatinine, Model for End-stage Liver Disease (MELD) score and body mass index (BMI). Donor factors included donor's age, BMI, degree of steatosis and graft to recipient weight ratio (GRWR). Among factors concerning donor-recipient interrelation, ABO blood type and HLA type (A, B and DR), donor-recipient relationship and the results of cytotoxicity tests were considered. Next, genetic information of donors' and recipients' own concerning KIRs and HLA-C allotypes were investigated. Because this information was not determined during the patient's admission, we asked recipients and their donors of that period to undergo an additional genetic test requiring a blood draw. Sixty-eight recipients and 59 donors gave informed consents and underwent the genetic test. Of them, those who have both their own and their donor's genetic information were 20 recipients. Recipient's genetic information was also compared with the control group (n=159) who are healthy Korean adults as volunteers (Table 1).
After transplantation, recipients received a quadruple immunosuppressive therapy consisting of calcineurin inhibitor (tacrolimus or cyclosporine), prednisone, mycophenolate mofetil (MMF) and IL-2 receptor antibody as induction therapy. Tacrolimus or cyclosporine comprised the mainstay of immunosuppression and the choice of tacrolimus or cyclosporine was randomized. The dose of calcineurin inhibitor was determined by the target level of drugs. Both MMF and prednisone were withdrawn by protocol as soon as possible; MMF was taken for about 1 month post-transplantation and steroid was gradually discontinued until 3 months post-transplantation.
To find the determinant factor(s) of the serum ALT pattern, researches were carried out into 2 ways: analysis of clinical variables including recipients', donors', their relations' aspect, and of genetic information including KIRs and their ligands.
The genotyping of HLA-C was performed by the amplification refractory mutation system-polymerase chain reaction (PCR) method.(15) Each reaction contained a primer mixture consisting of allele- or group-specific primer pairs as well as internal control primers matching nonallelic sequences. Specific amplification of the HLA-C gene was performed using 33 primers for HLA-C. PCR was carried out in a reaction (13µl) containing 100~200 ng genomic DNA, 0.8×buffer (40 mM KCl, 1.2 mM MgCl2, 8.0 mM Tris-HCl pH 8.8, 0.08% Triton X-100), 5% dimethyl sulfoxide (DMSO), 200µM of each dNTP, 0.25 U Taq DNA polymerase (Boehringer Mannheim, Germany), 1µM of each sequence-specific primer and 0.2µM of internal control primers. The amplifications were performed in a My Cycler™ thermocycler (Bio-Rad, CA, USA). A total of 30 cycles was used for the amplification with the following steps: heating to 96℃ for 1 min to denature the DNA, denaturation at 96℃ for 25 sec, annealing at 70℃ for 45 sec and extension at 72° for 30 sec (for the first 5 cycles); 96℃ for 25 sec, 65℃ for 45 sec, 72℃ for 30 sec (for the next 21 cycles); 96ofor 25 sec, 55℃ for 60 sec, 72℃ for 120 sec (for the last 4 cycles); and a final 1 min extension at 72℃. The presence or absence of PCR products was determined following separation on a 1.5% agarose gel containing 0.5 µg/ml ethidium bromide.
HLA-C alleles were assigned to HLA-C1 or HLA-C2 groups, as defined by KIR specificity; a donor or recipient who typed solely as C2 was referred to as homozygous for C2 alleles (genotype C2/C2) whereas an individual who typed as C1 alone was referred to homozygous for C1 alleles (genotype C1/C1). The remainders were described as C1/C2 heterozygotes.
The KIR alleles were determined by polymerase chain reaction using sequence-specific primers (PCR-SSP) methodology.(16) Inhibitory KIR were typed for KIR2DL1, KIR2DL2, KIR2DL3, KIR2DL4, KIR2DL5, KIR3DL1, KIR3DL2, and KIR3DL3 alleles, activating KIRs were typed for KIR2DS1, KIR2DS2, KIR2DS3, KIR2DS4, KIR2DS5 and KIR3DS1 alleles, and pseudo KIRs were typed for 2DP1 and 3DP1. Specific amplifications of the KIR genes were performed using 50 forward and reverse primers. PCR was carried out with primers in a reaction (10µl) containing 1×buffer, 0.1~0.5µM of each nucleotide primer, 2.5 mM dNTPs, 100 ng genomic DNA and 0.5 U Taq DNA polymerase (Boehringer Mannheim, Germany) The amplifications were carried out in a My Cycler™ thermocycler (Bio-Rad, CA, USA). A total of 35 cycles of PCR were completed using the following steps: 25 sec at 91℃, 45 sec at 65℃, 30 sec at 72℃ (first 4 cycles); 25 sec at 91℃, 45 sec at 60℃, 30 sec at 72℃ (next 26 cycles); 25 sec at 91℃, 60 sec at 55℃, 120 sec at 72℃ (last 5 cycles) and finally a 10-minute extension at 72℃. The presence or absence of PCR products was determined following separation on a 2% agarose gel containing 0.5µg/ml ethidium bromide.
All numerical data are described as the mean and standard error or as the median and range. Chi-square tests were used to compare the clinical parameters according to serum ALT pattern. Multiple regression analyses were performed using proportional hazards models to identify the factors independently associated with serum ALT pattern to estimate the corresponding relative risks (RR) in 95% confidence intervals. In comparing the numbers of KIRs, independent t-test and Chi-square test were utilized. Patient survival rates based on AR and serum ALT pattern were described with Kaplan-Meier curves and compared with the log-rank test. Statistical analysis was performed with SPSS (SPSS 15.0; SPSS Inc., Chicago, IL, USA) and results with a P value of <0.05 were considered significant.
A total of 319 patients undergoing adult LDLT using a right lobe were included in the cohort for this retrospective study. Of 115 patients who underwent liver biopsies under the impression of AR, 43 patients received the diagnosis of AR (43/115, 37.4%). Therefore, the actual incidence of histologically proven AR was 13.4% (43/319). Stratified by the serum ALT pattern, 184 (57.7%) patients were of a stable pattern and 135 (42.3%) patients were of an unstable pattern.
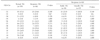
Factors affecting AR were the underlying disease of autoimmune and/or toxic hepatitis (P=0.020) and recipient's MELD score ≥25 (P=0.024) of which the latter was proved to be an independent risk factor through multivariate analysis (RR=2.489; 95% confidence interval (CI), 1.205~5.141; P=0.014). On the contrary, factors affecting unstable ALT pattern were the underlying disease of autoimmune and/or toxic hepatitis (P=0.001) and recipient's BMI ≥25 (P=0.001) of which the latter was proved to be an independent risk factor through multivariate analysis (RR=1.990; 95% CI, 1.198~3.305; P=0.008) (Table 2).
To investigate the influence of AR and serum ALT pattern on the immediate post-transplantation course, we examined their associations with post-transplantation complications. Post-transplantation complications were stratified according to Clavien's proposal.(17) Whereas no significant difference was found in the number of patients with total complications according to the presence of AR, statistical difference was detected in the groups stratified by serum ALT pattern; patients with unstable pattern appeared to have more complications than those with stable pattern (RR=1.667; 95% CI, 0.386~0.949; P=0.030). Next, to evaluate the effect of AR and serum ALT pattern on the short-term graft function, we compared the levels of serum AST, ALT, total bilirubin and albumin on 6 months post-transplantation according to each group. In recipients with AR and unstable ALT pattern as well, serum liver enzymes increased compared to those in recipients with non-AR and stable pattern, respectively (in non-AR vs. AR, AST, 44±2.4 vs. 68±7.5 IU/L (P=0.001), ALT 50±2.8 vs. 84±9.9 IU/L (P=0.039), total bilirubin 1.6±0.1 vs. 2.6±0.4 mg/dl (P=0.000); in stable vs. unstable pattern, in AST, 42±2.8 vs. 65±7.1 IU/L (P=0.001), ALT 53±3.9 vs. 69±7.3 IU/L (P=0.039) and total bilirubin 1.6±0.1 vs. 1.7±0.2 mg/dl (P=0.508)). For the investigation of the impact of AR and/or unstable ALT pattern on long-term patient survival, log-rank tests were used to compare Kaplan-Meier survival curves according to presence of AR and unstable ALT pattern. No survival differences were found according to the presence of AR (P=0.380). However, significant survival difference was detected according to serum ALT pattern; median overall survival was 71 months in patients with unstable ALT pattern, compared to 88 months for patients with stable ALT pattern (P=0.000)(Fig. 1).
Of 319 donor/recipient pairs, we could obtain genetic information of the KIR and HLA-C from 68 recipients and 59 donors. There were 20 cases in which genetic information for both recipient's and donor's was available. The comparison of HLA Cw* type was made, firstly between the control group and the patient group and next, between patients with stable and unstable ALT pattern (Table 3). In comparison between the control and the patients, the frequency of HLA Cw12 tended to be lower in the control group (11/159 [6.9%] versus 11/66 [16.2%]; P=0.047). However, between patients with stable and unstable ALT pattern, no significant difference was found.
Regarding the recipient's KIRs, certain differences were detected according to serum ALT pattern (Table 4). The frequency of KIR2DL2 in recipients with unstable ALT pattern was higher than that in recipients with stable ALT pattern (5/10 [50.0%] versus 8/56 [14.3%]; P=0.020). In addition, the frequency of KIR2DS2 was also higher in the unstable ALT pattern than the stable ALT pattern (6/10 [60.0%] versus 9/56 [16.1%]; P=0.007). We stratified the recipient population according to the recipient's HLA-C allotype. Three kinds of HLA-C allotype exist including HLA-C1/C1, HLA-C1/C2 and HLA-C2/C2. However, due to the paucity of recipients with HLA-C2/C2 (1/66, 1.5%) in our recipient population, the distributions of serum ALT pattern according to HLA-C1/C1 (homogenous) and HLA-C1/C2 (heterogeneous) were compared. There was no difference in the incidences of stable/unstable ALT pattern according to the HLA-C allotype (P=0.745). Furthermore, taking KIRs and HLA-C allotypes into consideration together, we investigated the risk factors affecting unstable ALT pattern (Fig. 2). When all recipients were considered, the relative risk of an unstable pattern was 6.0 times higher in recipients with KIR2DL2(+)/KIR2DS2(+) than in those with KIR2DL2(-) and/or KIR2DS2(-) (CI, 1.410~25.528; P=0.020). However, this difference became meaningless when compared in recipients with HLA-C1/C1 (P=0.583). In contrast, the relative risk increased up to 45 times when compared in recipients with HLA-C1/C2 (CI, 2.160~937.321; P=0.013). As a result, the unstable pattern seemed to exhibit its highest incidence in recipients with KIR2DL2(+)/KIR2DS2(+) combined with heterogeneous HLA-C (HLA-C1/C2).
AR is a well-characterized indicator of immunological consequences after LT. However, there have been several limitations of its application to assess graft function. The first is its lower incidence in LT compared to other transplantations and the next is the inability to define its exact incidence because AR necessitates invasive diagnostic procedure. In addition, under similar immunosuppressant dose regimens, certain patients showed stable biochemical parameters reflecting liver function during our follow-up period after LDLT, while others did not. These differences did not coincide with the episode or frequency of AR, causing us to assume that certain unknown factors besides AR might have played a role. Therefore, we introduced serum ALT pattern for assessing the graft function of the liver. Different from the magnitude of liver enzymes at a temporal point, the serum ALT pattern is the expression of stability of the liver condition throughout 3 months post-transplantation. Therefore, serum ALT pattern is expected to reflect the graft consequences after LT more precisely. In our study, serum ALT pattern was shown to be a stronger indicator as much as predicting post-transplantation survival than the presence of AR. Furthermore, when the withdrawal of immunosuppressant regimens is taken in consideration, decision making is based not on the presence or frequency of AR, but on the stability of liver function which the patients have exhibited so far. In this aspect, we think more attention should be paid to the clinical significance of serum ALT pattern.
Conventional immunology emphasizes the extraordinary work of T cells in the process of graft acceptance. Accordingly, T cells are considered to play a major role in the development of AR. However, several features such as the uselessness of strict matching of donor-recipient HLA types in selecting the transplant donor and the rather limited demand of immunosuppressant regimens in maintaining graft acceptance have led to the assumption that mechanisms besides T cell-centered immunity might have affected graft-host relationship.
Recently, the importance of KIRs has been highlighted after having realized their roles in various diseases related with immunity.(18-23) KIRs are involved in innate immunity through their effect on NK cells. In addition, KIRs have a role in acquired immunity because certain subsets of T cells express both them and TCR. Furthermore, it was reported that over 40% of lymphoid cells in the liver are NK cells whereas they comprise only 13% of peripheral blood.(24,25) Therefore, we began this study with the assumption that KIRs could have a role in LDLT immunology. Among KIRs, KIR2DL1, KIR2DL2 and KIR2DL3 bind their cognate HLA-C allotype C1 or C2 with different strengths.(7) In these combinations, KIR2DL1-HLA-C2 is known to provide the strongest inhibition of NK cell. Interactions of KIR2DL2-HLA-C1 and KIR2DL3-HLA-C2 follow in strength. Because a person carries several different KIRs, either activating or inhibitory, and there are 2 HLA-C haplotypes, HLA-C1 or HLA-C2, numerous combinations of KIR and HLA-C can develop exerting different strengths to NK cells. For example, KIR2DL1-HLA-C2/KIR2DL2-HLA-C1 exhibits stronger inhibition of NK cells than KIR2DL2-HLAC1/KIR2DL3-HLA-C1. On the other hand, KIR2DL3-HLA-C1/KIR2DL3-HLA-C1 exerts the weakest inhibition of NK cells.
Concerning the effects of KIRs and their ligands on LT, Moya-Quiles et al.(8) reported a high frequency of the HLA-C1 allotype and the relative lower incidence of HLA-Cw*05 allele in recipients without AR. They also stated that graft survival probability appeared to decrease with increasing numbers of mismatches in HLA-C types between the donor and recipient. Consequently, in their next report analyzing liver recipients, the protective effect of recipient HLA-Cw*07 against AR was also described.(26) Bishara et al.(27) also ascertained that the matched HLA-C compatibility in donor/recipient pairs significantly reduced the incidence of AR. Hanvesakul et al.,(28) after analyzing the liver donors at a single center, reported that the possession of at least one HLA-C2 allele by the donor allograft was associated with less histological evidence of chronic rejection and graft cirrhosis, reduction in graft loss and improvement in patient survival. This was attributed to the stronger NK cell inhibition provided by interaction between HLA-C2 and KIR2DL1 than by the interaction between HLA-C1 and KIR2DL2/3. However, the results was inconsistent in other report.(29) Tran et al.,(29) after analyzing the liver donors from multicenters, concluded that donor HLA-C2 genotype had no impact on 10-year graft or patient survival. The disparity between these 2 reports is thought to originate from several factors including group homogeneity, patient numbers and different genetic background.(30) As above, any results were not conclusive. Therefore, further and extensive studies are necessary to find the actual effect of the KIR-HLA ligand interaction between the donor and recipient.
In our analysis of KIRs and HLA-C types of the recipients, the incidence of unstable ALT pattern was highest in recipients with KIR2DL2(+)/KIR2DS2(+) combined with the heterogeneous HLA-C allotype (HLA-C1/C2). Our patient population exhibited ubiquitous presence of KIR2DL1 (56/56, 100.0%) and KIR2DL3 (55/56, 98.2%). As previously described, KIR2DL1/HLA-C2 (homogeneous) provides the strongest inhibition of NK cells, whereas the haplotypes of KIR2DL1/HLA-C2 and KIR2DL2/HLA-C1 provide the second. Because only 1 case of HLA-C2/C2 was observed in our study, if it were not, carrying the combination of haplotypes of KIR2DL1/HLA-C2 and KIR2DL2/HLA-C1 exerted the strongest inhibition of NK cells. Therefore, one possible explanation for the high incidence of unstable ALT pattern in recipients with KIR2DL2(+)/KIR2DS2(+) combined with HLA-C1/C2 is that the expression of KIR2DS2 in the background of forcefully inhibited NK cells (having KIR2DL1/HLA-C2 and KIR2DL2/HLA-C1) might destabilize immunologic function, resulting in unstable pattern.
We acknowledge that our study has several limitations. First, the small patient population, particularly in the genetic study, limits the generalization of the conclusion. Also, the patient population in the genetic study is likely to be biased; only 1 patient had a HLA-C2/C2 allotype. Next, our results were not based on a study composed of well-matched donor/recipient pairs. Therefore, the possible effect between the donor's HLC-C and recipient's KIRs, which might have affected the serum ALT pattern by way of direct allorecognition, was not taken into account. Our results should be confirmed by a study based on large-scale population composed of well-matched donor/recipient pairs. Despite these shortcomings, we think our results are worth considering as they suggest the presence of genetically fragile recipients who could exhibit an immunologically unstable clinical course after transplantation.
Briefly, in addition to the presence of AR, serum ALT pattern could be utilized as a surrogate of post-transplantation immunological consequences and, different from AR, it correlated with post-transplant patient survival. The unstable ALT pattern was related to recipients carrying KIR2DL2(+)/KIR2DS2(+) combined with the heterogeneous HLA-C allotype (HLA-C1/C2). Our results suggest that, in the process of graft acceptance, besides interaction between the T cells and APCs, KIRs and their ligands (HLA-C) might have played an important role. Although more extensive studies are needed to confirm our results, this study documents that, in performing LDLT, pretransplant determination of the recipient's KIRs and HLA-C allotypes combined with expectant management according to the genetic background can be useful in coping with post-transplant immunological circumstances.
Figures and Tables
 | Fig. 1Survival curves in each group stratified according to presence of acute rejection and serum ALT pattern and acute rejection. (A) Overall survival according to presence of acute rejection, (B) Overall survival according to serum ALT pattern. |
 | Fig. 2Distributions of stable/unstable pattern according to the recipient's HLA-C allotypes in patients with KIR2DL2(+)/KIR2DS2(+). |
Table 2
Univariate analysis of the factors affecting groups stratified according to serum ALT* pattern

ACKNOWLEDGEMENTS
This study was supported by a grant of the Korea Healthcare technology R&D Project, Ministry for Health, Welfare&Family Affairs, Republic of Korea. (No.: A092258) and Novartis Co (No.: 5-2006-D0227-00002).
References
1. Mazariegos GV, Reyes J, Marino IR, Demetris AJ, Flynn B, Irish W, et al. Weaning of immunosuppression in liver transplant recipients. Transplantation. 1997. 63:243–249.
2. Sandborn WJ, Hay JE, Porayko MK, Gores GJ, Steers JL, Krom RA, et al. Cyclosporine withdrawal for nephrotoxicity in liver transplant recipients does not result in sustained improvement in kidney function and causes cellular and ductopenic rejection. Hepatology. 1994. 19:925–932.
3. Golling M, Frankenberg MV, Hofmann WJ, Lohse A, Herfarth C, Otto G. Cyclosporine A reduction and withdrawal in liver transplantation: a risk-benefit analysis. Transplant Proc. 1997. 29:2819–2821.
4. Devlin J, Doherty D, Thomson L, Wong T, Donaldson P, Portmann B, et al. Defining the outcome of immunosuppression withdrawal after liver transplantation. Hepatology. 1998. 27:926–933.
5. Takatsuki M, Uemoto S, Inomata Y, Egawa H, Kiuchi T, Fujita S, et al. Weaning of immunosuppression in living donor liver transplant recipients. Transplantation. 2001. 72:449–454.
6. Vilches C, Parham P. KIR: diverse, rapidly evolving receptors of innate and adaptive immunity. Annu Rev Immunol. 2002. 20:217–251.
7. Parham P. MHC class I molecules and KIRs in human history, health and survival. Nat Rev Immunol. 2005. 5:201–214.
8. Moya-Quiles MR, Muro M, Torio A, Sanchez-Bueno F, Miras M, Marin L, et al. Human leukocyte antigen-C in short- and long-term liver graft acceptance. Liver Transpl. 2003. 9:218–227.
9. Moretta A, Biassoni R, Bottino C, Pende D, Vitale M, Poggi A, et al. Major histocompatibility complex class I-specific receptors on human natural killer and T lymphocytes. Immunol Rev. 1997. 155:105–117.
10. Vivier E, Anfossi N. Inhibitory NK-cell receptors on T cells: witness of the past, actors of the future. Nat Rev Immunol. 2004. 4:190–198.
11. Boyington JC, Brooks AG, Sun PD. Structure of killer cell immunoglobulin-like receptors and their recognition of the class I MHC molecules. Immunol Rev. 2001. 181:66–78.
12. Biassoni R, Falco M, Cambiaggi A, Costa P, Verdiani S, Pende D, et al. Amino acid substitutions can influence the natural killer (NK)-mediated recognition of HLA-C molecules. Role of serine-77 and lysine-80 in the target cell protection from lysis mediated by "group 2" or "group 1" NK clones. J Exp Med. 1995. 182:605–609.
13. Demetris AJ, Seaberg EC, Batts KP, Ferrell LD, Ludwig J, Markin RS, et al. Reliability and predictive value of the National Institute of Diabetes and Digestive and Kidney Diseases Liver Transplantation Database nomenclature and grading system for cellular rejection of liver allografts. Hepatology. 1995. 21:408–416.
14. Ormonde DG, de Boer WB, Kierath A, Bell R, Shilkin KB, House AK, et al. Banff schema for grading liver allograft rejection: utility in clinical practice. Liver Transpl Surg. 1999. 5:261–268.
15. Bunce M, Welsh KI. Rapid DNA typing for HLA-C using sequence-specific primers (PCR-SSP): identification of serological and non-serologically defined HLA-C alleles including several new alleles. Tissue Antigens. 1994. 43:7–17.
16. Gomez-Lozano N, Vilches C. Genotyping of human killer-cell immunoglobulin-like receptor genes by polymerase chain reaction with sequence-specific primers: an update. Tissue Antigens. 2002. 59:184–193.
17. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004. 240:205–213.
18. Hiby SE, Walker JJ, O'Shaughnessy KM, Redman CW, Carrington M, Trowsdale J, et al. Combinations of maternal KIR and fetal HLA-C genes influence the risk of preeclampsia and reproductive success. J Exp Med. 2004. 200:957–965.
19. Ruggeri L, Capanni M, Mancusi A, Martelli MF, Velardi A. The impact of donor natural killer cell alloreactivity on allogeneic hematopoietic transplantation. Transpl Immunol. 2005. 14:203–206.
20. Suzuki Y, Hamamoto Y, Ogasawara Y, Ishikawa K, Yoshikawa Y, Sasazuki T, et al. Genetic polymorphisms of killer cell immunoglobulin-like receptors are associated with susceptibility to psoriasis vulgaris. J Invest Dermatol. 2004. 122:1133–1136.
21. van der Slik AR, Koeleman BP, Verduijn W, Bruining GJ, Roep BO, Giphart MJ. KIR in type 1 diabetes: disparate distribution of activating and inhibitory natural killer cell receptors in patients versus HLA-matched control subjects. Diabetes. 2003. 52:2639–2642.
22. Cook MA, Milligan DW, Fegan CD, Darbyshire PJ, Mahendra P, Craddock CF, et al. The impact of donor KIR and patient HLA-C genotypes on outcome following HLA-identical sibling hematopoietic stem cell transplantation for myeloid leukemia. Blood. 2004. 103:1521–1526.
23. Momot T, Koch S, Hunzelmann N, Krieg T, Ulbricht K, Schmidt RE, et al. Association of killer cell immunoglobulin-like receptors with scleroderma. Arthritis Rheum. 2004. 50:1561–1565.
24. Doherty DG, Norris S, Madrigal-Estebas L, McEntee G, Traynor O, Hegarty JE, et al. The human liver contains multiple populations of NK cells, T cells, and CD3+CD56+ natural T cells with distinct cytotoxic activities and Th1, Th2, and Th0 cytokine secretion patterns. J Immunol. 1999. 163:2314–2321.
25. Liu ZX, Govindarajan S, Okamoto S, Dennert G. NK cells cause liver injury and facilitate the induction of T cell-mediated immunity to a viral liver infection. J Immunol. 2000. 164:6480–6486.
26. Moya-Quiles MR, Alvarez R, Miras M, Gomez-Mateo J, Lopez-Alvarez MR, Marin-Moreno I, et al. Impact of recipient HLA-C in liver transplant: a protective effect of HLA-Cw*07 on acute rejection. Hum Immunol. 2007. 68:51–58.
27. Bishara A, Brautbar C, Zamir G, Eid A, Safadi R. Impact of HLA-C and Bw epitopes disparity on liver transplantation outcome. Hum Immunol. 2005. 66:1099–1105.
28. Hanvesakul R, Spencer N, Cook M, Gunson B, Hathaway M, Brown R, et al. Donor HLA-C genotype has a profound impact on the clinical outcome following liver transplantation. Am J Transplant. 2008. 8:1931–1941.
29. Tran TH, Middleton D, Dohler B, Scherer S, Meenagh A, Sleator C, et al. Reassessing the impact of donor HLA-C genotype on long-term liver transplant survival. Am J Transplant. 2009. 9:1674–1678.
30. Mendel JB, Chavin KD, Bratton C, Knechtle SJ. HLA-C and liver transplant outcomes: interpreting the facts. Am J Transplant. 2009. 9:1491–1492.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download