Abstract
Purpose
This study is to introduce our preliminary experience of the Doppler-guided hemorrhoidal artery ligation and Rectoanal repair (DG-HAL & RAR) as a new treatment for symptomatic or prolapsed hemorrhoids.
Methods
A Doppler probe incorporated proctoscope was inserted under the lithotomy position and the location of the hemorrhoidal artery was identified. The identified artery was ligated as a 'figure of eight' method with an absorbable suture into the submucosa. Then the prolapsed hemorrhoidal pile was lifted at the rectal mucosa by continuous suture to 5 mm above the dentate line and tied. The procedure was repeated at the 1, 3, 5, 7, 9, and 11 o'clock positions. We evaluated post-operative hospital stay, degree of pain, time to return to work, and recurrence.
Results
The patient's mean age was 50.2±15 years old and the mean follow-up time was 415±75 days. The constitution of the type of internal hemorrhoids was as follows: Grade II: 13, Grade III: 16, and Grade IV: 5. The mean operation time was 35 minutes and post-operative hospital stay was 1.4 days. The mean time it took to return to work was 1.8 days. There were no severe pains requiring injection of analgesics or other severe complications. So far, 2 patients have had recurrence of symptoms.
Since Dr. Morinaga first introduced a method of treatment for hemorrhoids by using a Doppler scope to find and ligate the vessels supplying the hemorrhoidal pile (Doppler-guided hemorrhoidal artery ligation, DG-HAL) in 1995, there have been many studies about this technique.(1)
As most studies report that the DG-HAL results in minimal post operative pain with less than 10% recurrence rate and over 90% patient satisfaction, it is being widely used in Europe and Japan as an alternative procedure to conventional hemorrhoidectomy.(1-3)
However, most of studies have been based on Grade II and III internal hemorrhoids that show the symptoms of bleeding and discomfort.(4) As for symptomatic Grade IV hemorrhoids with prolapse, the DG-HAL has its limitations. With the DG-HAL, symptoms such as bleeding may improve shortly after surgery. But the improvement of prolapse is difficult as it takes long time for the hemorrhoidal pile to shrink. Also, this treatment is difficult to apply to the prolapsed cases occurred by the destruction of anchoring connective tissue in the anal cushion.
We tried combining mucopexy (Recto-anal repair, RAR) with the DG-HAL as a treatment procedure for such symptomatic hemorrhoids and describe the results of the DG-HAL & RAR technique.
Thirty four patients who underwent the DG-HAL & RAR after being diagnosed with hemorrhoids at our institution from November 2007 to March 2009 were prospectively analyzed. Surgical indications were Grade II-IV internal hemorrhoids with symptoms of bleeding, prolapse, or pain. Patients with other anal problems such as anal fistulas or anal fissures were excluded from this study. Most of patients underwent spinal anesthesia, but some underwent general anesthesia according to the patient's preferences. Patients were placed in the lithotomy position during surgery.
First, an anoscope with an incorporated Doppler probe was inserted into the anus with a specially made sleeve, and the superior hemorrhoidal artery was identified with the Doppler probe (Fig. 1). The detection of the branch of the superior hemorrhoidal artery was confirmed by a sound from the Doppler probe and an image display on the monitor. Ligation of the artery was carried out through the window of the anoscope with a figure-of-eight suture using vicryl #2-0. Correct ligation of the artery was confirmed by absence of the Doppler sound, and a knot-pusher was used to tie a knot. Up to this point, the surgery is identical to the DG-HAL procedure.
After ligation of the artery, the anoscope was repositioned to expose the prolapsed hemorrhoidal pile through the space between the anoscope and sleeve. Continuous running suture using vicryl #2-0 was performed from the location of hemorrhoidal artery ligation to 5 mm above the dentate line and then tied in order to lift the hemorrhoidal pile towards the rectal mucosa, correcting the prolapsed (Fig. 2). The same procedure was repeated in 6 positions (1, 3, 5, 7, 9, 11 o'clock) of the anus. The surgery was terminated after confirming no more prolapsed hemorrhoidal pile.
We evaluated postoperative hospital stay, degree of pain, operation time, recovery time that patient goes back to normal life, complications, and recurrence. Preoperative and postoperative pain was compared using a 10-point pain scale (0 = no pain; 10 = extremely painful). We also asked the degree of satisfaction with the operation results and whether they would recommend this procedure to others.
Of 34 patients, 18 were male and 16 were female. The mean age was 50.2±15 (20~86) years old. Thirteen patients had Grade II, 16 had Grade III, and 5 had Grade IV internal hemorrhoids according to Goligher classification. The mean follow-up duration was 415±75 days. The mean time of operation was 35 minutes, and mean postoperative hospital stay was 1.4 days. Most patients were able to return to work 1.8±1.4 days after the operation.
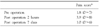
Before the operation, the mean pain score was 1.8 (0~7). After 2 hours of surgery, the mean pain score was 3.9 (0~8). But after 7 days of surgery, the mean pain score decreased to 1.0 (0~6) and this was mostly controlled by oral analgesics without difficulties in everyday life (Table 1). Postoperative complications were recorded in 2 patients; one is urinary retention in Grade II and the other is postoperative bleeding in Grade III. However, both patients improved with conservative treatment.
When we asked the patients the degree of satisfaction with the operation results and whether they would recommend the surgery to others, taking into consideration the postoperative pain and surgical results, 31 out of the 34 patients (91%) said that they were satisfied and would recommend the DG-HAL & RAR to others.
Until now, 2 patients with Grade IV internal hemorrhoids had recurrence of prolapse.
As for the patients with Grade II, III internal hemorrhoids, there has been no recurrence of symptoms so far (Fig. 3).
The conservative treatment such as rubber band ligation and sclerotherapy have been developed for the treatment of Grade I and II hemorrhoids with light symptoms or no prolapsed, and have shown good results.
As for Grade III and IV hemorrhoids with prolapse or severe symptoms, Milligan-Morgan's open hemorrhoidectomy, Ferguson's closed hemorrhoidectomy or other variants of these procedures have been used as primary treatment for a long time. However, these surgical procedures create postoperative pain and it takes a long time for the patients to return to work. For this reason, many patients with advanced hemorrhoids hesitate in making a decision to undergo surgery.
As the pathogenesis of hemorrhoids have been identified as abnormal dilatation of the veins of the internal hemorrhoidal venous plexus, abnormal distention of the arteriovenous anastomosis, and downward displacement or prolapse of the anal cushion, surgical procedures that take these into consideration and minimize postoperative pain and enable quick return to work have been developed. The stapled hemorrhoidectomy (PPH) and the doppler-guided hemorrhoidal artery ligation are the less invasive surgical procedures for hemorrhoids.(1-3,5)
The Doppler-guided hemorrhoidal artery ligation was introduced in 1995 by Dr. Morinaga in Japan for the first time. An anoscope with an incorporated Doppler probe is used to accurately detect the branch from the superior rectal artery that supplies the hemorrhoidal pile. The vessel is then ligated in order to induce shrinkage of the hemorrhoidal mass.(6)
Wallis de Vries et al.(7) treated 42 Grade II and 68 Grade III hemorrhoid patients with the DG-HAL, and reported that 88% of the treated patients showed improved symptoms and 85% expressed satisfaction with the results and post operative course. Nine percent of the treated patients were re-treated, and 6% complained of immediate postoperative pain that interfered with returning to work.
As there are no long-term follow up results of the DG-HAL compared to conventional hemorrhoidectomy, some express negative views on the DG-HAL. However, Bursics et al.(8) reported that there was no difference in recurrence of preoperative symptoms between hemorrhoidectomy and DG-HAL after a 1 year follow up period. Also, Faucheron and Gangner(4) reported that out of 100 patients (Grade II-1, Grade III-78, Grade IV-21) that underwent DG-HAL, 12% recurred after a follow up period of 3 years.
But, though the DG-HAL shows good results for many cases of hemorrhoids, this treatment is difficult to apply to the prolapsed cases occurred by the destruction of anchoring connective tissue in the anal cushion.
There are many studies that report that it is possible to correct prolapse by mucopexy.
In 2001, Hussein(9) first announced the results of ligation & anopexy for the treatment of advanced hemorrhoids. The method is similar to the DG-HAL & RAR, but instead of using a Doppler probe for hemorrhoidal artery ligation, the hemorrhoidal pile, identified by the naked eye, is reduced into the anal canal and the mucosa and submucosa, which are fixed onto the underlying internal sphincter. The objects of Hussein's study were 22 Grade III and 18 Grade IV internal hemorrhoid patients, and after a 12 month follow up period, no recurrences or anal stenosis were reported. Although artery ligation was not appropriately carried out, this study showed that symptoms of prolapse can be improved by mucopexy alone.
Gupta also reported that correction of hemorrhoids is possible by using radiofrequency ablation on the hemorrhoidal pedicle and oversewing the hemorrhoidal mass with absorbable suture after analyzing 410 Grade III and IV hemorrhoid patients with major complaints of severe prolapse symptoms who underwent his procedure.(10, 11) As above, our study got good operative results by combing mucopexy with the DG-HAL.
Aigner et al.(12) studied the possibility of hemorrhoidal pile shrinkage by DG-HAL alone through an anatomical study of 38 cases. This study showed that the ligation of the main trunk of the superior rectal artery (SRA) was possible by the DG-HAL technique, which can ligate a vessel 3 cm above the dentate line, but that interruption of the additional branch of the SRA which supplies the corpus cavernosum recti (CCR) by piercing the muscular layer of the rectal wall was difficult. For this reason, he explained that hemorrhoids may persist after ligation using the DG-HAL. However, if mucopexy is performed at the same time, interruption of the CCR or even the branch of the middle rectal artery by running suture can be possible. Therefore, not only can we correct prolapse, but we can also induce shrinkage of the hemorrhoidal pile more effectively compared to when using the DG-HAL alone. As shown above, although the results of the treatment of symptomatic hemorrhoids by the DG-HAL alone are effective, combining mucopexy may help reduce pain in treating advanced hemorrhoids (Grade IV) with main symptoms of prolapse or anal mucosa sliding.
As multiple sutures and ligations are performed within the anal canal, it is natural to be concerned about the change in sphincter or anal function.
Walega et al.(13) studied the possible change of anal function after the DG-HAL using anal manometry. Although conventional hemorrhoidectomy influences sphincter function, Walega's study showed that after the DG-HAL, the basal anal pressure, squeeze pressure, vector volume, and radial asymmetry function of the anus showed no significant difference compared to before the surgery. In our study, there is no one who complained of tenesmus, or sphincter dysfunction.
Although concurrent removal of skin tags is not possible as in conventional hemorrhoidectomy, skin tags are different from hemorrhoids and they do not generate pain nor are they painful after removal. Arnold et al.(14) also reported that the remaining anodermal fold after the DG-HAL can easily be removed with local anesthesia.
The merit of this procedure is that it is possible for the patients to return to daily life more quickly. Most patients replied that they returned to daily life in an average of 2 days after surgery, and pain control was possible with oral analgesics such as diclofenac with no complaints of large discomfort. Although a direct comparison to other paper is a stretch, many studies report that patients who received stapled hemorrhoidectomy returned to daily life in an average of 8 to 14 days, and those who received open hemorrhoidectomy took a longer 10 to 24 days.(15-18)
The DG-HAL & RAR is a safe and less painful procedure and it makes patients return to work more quickly. Also, the DG-HAL & RAR procedure can correct symptomatic, prolapsed (Grade II~IV) hemorrhoids with satisfactory results, which is difficult with DG-HAL alone. Therefore, we think the DG-HAL & RAR is an effective alternative for the treatment of symptomatic, prolapsed (Grade II~IV) hemorrhoids.
However, since the follow-up period was short and the number of samples was relatively small, we assume that long-term follow-up of enough samples is required in the future. Furthermore this study should be developed in comparison with other surgical procedures that are currently used.
Figures and Tables
References
1. Felice G, Privitera A, Ellul E, Klaumann M. Doppler-guided hemorrhoidal artery ligation: an alternative to hemorrhoidectomy. Dis Colon Rectum. 2005. 48:2090–2093.
2. Scheyer M, Antonietti E, Rollinger G, Mall H, Arnold S. Doppler-guided hemorrhoidal artery ligation. Am J Surg. 2006. 191:89–93.
3. Greenberg R, Karin E, Avital S, Skornick Y, Werbin N. First 100 cases with Doppler-guided hemorrhoidal artery ligation. Dis Colon Rectum. 2006. 49:485–489.
4. Faucheron JL, Gangner Y. Doppler-guided hemorrhoidal artery ligation for the treatment of symptomatic hemorrhoids: early and three-year follow-up results in 100 consecutive patients. Dis Colon Rectum. 2008. 51:945–949.
5. Longo A. Treatment of hemorrhoidal disease by reduction of mucosa and hemorrhoidalprolapse with a circular suturing device: a new procedure. 1998. In : Proceedings of 6th World Congress of Endoscopic Surgery; Jun 3~6; Rome, Italy: 777–784.
6. Morinaga K, Hasuda K, Ikeda T. A novel therapy for internal hemorrhoids: ligation of the hemorrhoidal artery with a newly devised instrument (Moricorn) in conjunction with a Doppler flowmeter. Am J Gastroenterol. 1995. 90:610–613.
7. Wallis de Vries BM, van der Beek ES, de Wijkerslooth LR, van der Zwet WC, van der Hoeven JA, Eeftinck Schattenkerk M, et al. Treatment of grade 2 and 3 hemorrhoids with Doppler-guided hemorrhoidal artery ligation. Dig Surg. 2007. 24:436–440.
8. Bursics A, Morvay K, Kupcsulik P, Flautner L. Comparison of early and 1-year follow-up results of conventional hemorrhoidectomy and hemorrhoid artery ligation: a randomized study. Int J Colorectal Dis. 2004. 19:176–180.
9. Hussein AM. Ligation-anopexy for treatment of advanced hemorrhoidal disease. Dis Colon Rectum. 2001. 44:1887–1890.
10. Gupta PJ. Hemorrhoidal ablation and fixation: an alternative procedure for prolapsing hemorrhoids. Digestion. 2005. 72:181–188.
11. Gupta PJ. Radioablation and suture fixation of advance grades of hemorrhoids. An effective alternative to staplers and Doppler guided ligation of hemorrhoids. Rev Esp Enferm Dig. 2006. 98:740–746.
12. Aigner F, Bodner G, Conrad F, Mbaka G, Kreczy A, Fritsch H. The superior rectal artery and its branching pattern with regard to its clinical influence on ligation techniques for internal hemorrhoids. Am J Surg. 2004. 187:102–108.
13. Walega P, Scheyer M, Kenig J, Herman RM, Arnold S, Nowak M, et al. Two-center experience in the treatment of hemorrhoidal disease using Doppler-guided hemorrhoidal artery ligation: functional results after 1-year follow-up. Surg Endosc. 2008. 22:2379–2383.
14. Arnold S, Antonietti E, Rollinger G, Scheyer M. Doppler ultrasound assisted hemorrhoid artery ligation. A new therapy in symptomatic hemorrhoids. Chirurg. 2002. 73:269–273.
15. Huang WS, Chin CC, Yeh CH, Lin PY, Wang JY. Randomized comparison between stapled hemorrhoidopexy and Ferguson hemorrhoidectomy for grade III hemorrhoids in Taiwan: a prospective study. Int J Colorectal Dis. 2007. 22:955–961.
16. Bikhchandani J, Agarwal PN, Kant R, Malik VK. Randomized controlled trial to compare the early and mid-term results of stapled versus open hemorrhoidectomy. Am J Surg. 2005. 189:56–60.
17. Wang JY, Lu CY, Tsai HL, Chen FM, Huang CJ, Huang YS, et al. Randomized controlled trial of LigaSure with submucosal dissection versus Ferguson hemorrhoidectomy for prolapsed hemorrhoids. World J Surg. 2006. 30:462–466.
18. Gravie JF, Lehur PA, Huten N, Papillon M, Fantoli M, Descottes B, et al. Stapled hemorrhoidopexy versus milliganmorgan hemorrhoidectomy: a prospective, randomized, multicenter trial with 2-year postoperative follow up. Ann Surg. 2005. 242:29–35.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download