Abstract
Purpose
Conventional three-port laparoscopic appendectomy (LA) is more commonly performed than transumbilical single port laparoscopic appendectomy (TUSPLA). In this report, we performed a prospective randomized study comparing the outcomes of LA and TUSPLA.
Methods
Between April 14, 2009 and June 10, 2009, 40 patients who required laparoscopic appendectomies were randomly selected to receive either a TUSPLA or a LA. None of these patients had perforation or abscess. Twenty of the patients received a LA and the other 20 received a TUSPLA. The clinical outcomes and visual analog pain scores (VAS) were compared between the groups.
Appendicitis is the most common intra-abdominal condition requiring emergency surgery and carries a lifetime risk of 6%.(1,2) For more than a century, open appendectomy remained the gold standard for the treatment of acute appendicitis.
Semm(3) described the first endoscopic appendectomy in early 1983. Laparoscopic surgery has become popular in developed countries during the last decade primarily because it is associated with improved cosmetic results, shorter hospital stays, less postoperative pain, and earlier return to work. However, despite these advantages, efforts are still being made to decrease abdominal incision and visible scars after laparoscopy. The use of technology to accomplish "scarless" surgery may eventually give rise to a new paradigm of disease management-based patient care. Recent research has led to the development of natural orifice translumenal endoscopic surgery (NOTES). However, there are numerous difficulties that need to be overcome before the wider clinical application of NOTES is adopted, including complications such as the opening of hollow viscera with associated risk of peritonitis, failed sutures, and pneumoperitoneum; a lack of fully developed instrumentation; and the necessity of reliable cost-benefit analyses.(4-7)
Transumbilical single port laparoscopic surgery is virtually scarless as the intra-abdominal entry point is hidden in the umbilicus. This procedure is becoming a common alternative form of minimally invasive surgery. Since 1992, after the initial performance of a single-trocar appendectomy,(8) various studies evaluating transumbilical single-port laparoscopic appendectomies (TUSPLA) have been conducted.(9-12) However, until recently TUSPLA has been less popular in clinical practice than traditional laparoscopic appendectomy (LA). The goal of our study was to conduct a comparative analysis of the clinical outcomes for LA and TUSPLA.
Between April 14, 2009 and June 10, 2009, 123 patients were diagnosed with acute appendicitis at Kangdong Sacred Heart Hospital. The diagnoses were made using physical examinations, laboratory studies, and imaging studies (abdominal ultrasonography and abdominal-pelvic computed tomography). All patients required and underwent a surgical operation. Seventy one patients with the following conditions were excluded from the study sample: a history of cirrhosis or coagulation disorders, shock on admission, a large ventral hernia, history of laparotomy, severe cardiac or pulmonary disease, mental disability, and pregnancy. The risks and benefits of the two types of surgeries, including costs, were explained to the patients and asked to sign a detailed informed consent approved by institutional review board (IRB). Five patients did not give their consent to enroll in the study and 2 patients were lost during followup. Five patients were excluded because they were suspected to have complicated appendicitis. This included a perforated appendix or periappendiceal abscess detected by physical examination, laboratory data (WBC>20,000), or imaging studies. Forty qualified patients were ultimately enrolled in the study (Fig. 1). Twenty patients were randomly assigned to the LA group, and 20 to the TUSPLA group.
All of the operations included in this study were performed by a single surgeon, who has completed over 100 laparoscopic appendectomies. For the TUSPLA procedures, a surgical glove was used as the single port with an extra-small wound retractor (ALEXIS wound retractor XS®, Applied Medical, Rancho Santa Margarita, CA, USA) set up through a small umbilical incision. The surgical glove was attached using three trocars that were fixed to the outer ring of the wound retractor. A 5 mm grasper (Roticulator EndoGrasp®, Covidien, Autosuture, Hamilton, Bermuda) was used to retract the appendix. The LA procedures were performed using a conventional three port technique (two 5 mm trocars and a 10 mm trocar). For both operation methods, we routinely used harmonic scalpels or endoclips to control the mesoappendix and an endo-loop (SJ Medical, Paju, Korea) to occlude the appendix stump.
A second generation cephalosporin was immediately administered as soon as a diagnosis of appendicitis was made. This therapy was continued until postoperative day 1.
The white blood cell count and C-reactive protein were measured preoperatively, at the time of diagnosis, and again on postoperative day 3.
The entire operative time from the skin incision to the last stitch was measured to the minute.
Time from the first gas out after the completion of the operation, as well as the first oral intake was measured to the hour.
Postoperative pain was assessed in two ways. A 10 cm visual analog pain score (VAS) with options ranging from 0 (no pain) to 10 (worst pain imaginable) was recorded by the patients four times per day until postoperative day 2. The VAS was completed by the patient just after waking up in the morning, at noon, at 6 PM, and before going to sleep. It was checked twice per day by the medical team. Ketoprofen 100 mg and Tramadol 50 mg were given until postoperative day 2. We recorded whenever patients asked for painkillers due to postoperative pain.
The outcomes for the patients who received a simple appendectomy were evaluated by doctors on postoperative day 3. The criteria that were used to determine postoperative outcomes included physical well-being, tolerance of a normal diet, and laboratory results. The postoperative hospital stay was then checked and recorded.
The results for the two groups were compared using an unpaired t-test and a chi-square analysis. A P-value of less than 0.05 was considered statistically significant. The SPSS 13.0 software package (Statistical Package for the Social Sciences, Chicago, IL, USA) was used for the statistical calculations.
The two patient groups included in this study did not differ in terms of age, sex, initial WBC, or initial CRP (Table 1). The operating time was shorter for the LA patients (54.0±12.5 min) than the TUSPLA patients (63.5±13.2 min). However, this difference was not statistically significant. Postoperative day 3 WBC and CRP levels, time until gas out, diet, and length of postoperative hospital stay were similar in both study groups. Patients in the two groups were equally satisfied with their cosmetic results (P=0.759)(Table 2). The TUSPLA group reported a significantly higher average VAS score than the LA group (P<0.05) during the first 24 postoperative hours (Fig. 2). There were no differences in the amounts of IV pain control that were used during hospitalization (P=0.543).
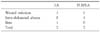
Complications occurred in four patients. In the LA group, one patient had a wound infection, and another had paralytic ileus. In the TUSPLA group, one patient had a wound infection, and another had an intra-abdominal abscess (Table 3). The patient who had ileus in the LA group resolved after three days fasting and was discharged from the hospital. The patient who had the intra-abdominal abscess in the TUSPLA group was diagnosed in the outpatient clinic on postoperative day 7 and admitted. The abscess resolved after seven days of antibiotic therapy, and the patient was then discharged from the hospital. One patient in the TUSPLA group was found to have a perforated appendix during surgery. A 5 mm trocar was added to the supra-pubic lesion and a drain was inserted.
Minimally invasive surgery is becoming very popular. In 2004, Kalloo et al.(13) published a study on the endoscopic scanning of the internal abdominal cavity after an abdominal wall incision. Since then, various studies on NOTES have been conducted. NOTES is a new operative technology that does not involve a skin incision. Clinical trials have been conducted on small end organ procedures including appendectomies, cholecystectomies, as well as on large organs such as the colon.(13-19) However, clinical trials involving NOTES have not been conducted frequently on human subjects. There are many obstacles that need to be overcome before NOTES is widely performed.(4-7)
TUSPLA has the advantage of requiring only a single incision in the umbilicus, making it virtually scarless. It is easily compared to NOTES, and is thus becoming more popular. The TUSPLA technique using a wound retractor and glove that was originally presented by Hong et al.(20) may be performed with conventional instruments without extra cost. Our hospital has been performing TUSPLA since 2009.
Our study was conducted safely and showed no differences in clinical outcomes between patients treated by TUSPLA and LA. These results are similar to those of previous studies.(11,20) If necessary, a surgeon can easily convert a TUSPLA procedure to a LA by adding another trocar. This allows the safety of the patient to be preserved.
The TUSPLA group in our study suffered from several disadvantages. A previous study found no differences in the VAS measurements between patients treated by LA and TUSPLA one day after the operation.(11) However, that study did not conduct successive postoperative VAS measurements. In the results of the present study, serial examination of post-operative pain intensity by VAS documented significantly higher levels of pain in TUSPLA patients 24 hours after surgery. This may have been caused by the length of the fascial incision, which is longer than that of umbilical incision used in a TULA, and the wound irritation seemed to be greater when the surgical instrument had to be inserted through only single incision. The bladeless trocars that are currently being used for TUSPLA minimize injury to the abdominal wall tissue. This could be a factor which leads to differences in reported pain between the two groups.(21-23)
As previously mentioned, the external instrument clashing and limitation of motion that is caused by the parallel and close proximity of the instruments that must operate through one small hole are problems that could be solved by instrument development.(11,20,24,25)
There were some limitations to this study. The average age of the LA and TUSPLA group was younger, and the number of female patients was higher compared to that of the entire population that was diagnosed with appendicitis during the same period (26.1 vs. 32.0, 57.5% vs. 43%). This reflects the fact that patients who preferred laparoscopic operations and young female patients who were sensitive to scarring, were more likely to be enrolled in the study.
Based on the preoperative evaluations, those patients who were suspected of having complicated appendicitis, such as an abscess or perforation, were exempted from the study. To overcome this limitation, a study with a larger sample of patients with appendicitis included abscess and perforation should be carried out.
TUSPLA is a "scarless" operation. The questionnaire administered during this study revealed no differences in satisfaction with scarring between the two groups (P=0.759). The TUSPLA patients did not have the chance to compare their scars with those created by different operation methods. Consequently, a different method of conducting the satisfaction survey is required for more objectivity.
In conclusion, Compared to LA, TUSPLA was technically feasible and safe in patients with non-complicated appendicitis. Considering the risks and benefits of TUSPLA that were discussed in this study, more careful patient selection is necessary. Further prospective studies comparing TUSPLA and LA in a large number of patients, especially for pain evaluation, including those with complicated appendicitis, are required to confirm the current promising results.
Figures and Tables
References
1. Samelson SL, Reyes HM. Management of perforated appendicitis in children--revisited. Arch Surg. 1987. 122:691–696.
2. A sound approach to the diagnosis of acute appendicitis. Lancet. 1987. 1:198–200.
3. Semm K. Endoscopic appendectomy. Endoscopy. 1983. 15:59–64.
4. Pearl JP, Ponsky JL. Natural orifice translumenal endoscopic surgery: a critical review. J Gastrointest Surg. 2008. 12:1293–1300.
5. Palanivelu C, Rajan PS, Rangarajan M, Parthasarathi R, Senthilnathan P, Praveenraj P. Transumbilical flexible endoscopic cholecystectomy in humans: first feasibility study using a hybrid technique. Endoscopy. 2008. 40:428–431.
6. Varas Lorenzo MJ, Espinos Perez JC, Bardaji Bofill M. Natural orifice transluminal endoscopic surgery (NOTES). Rev Esp Enferm Dig. 2009. 101:275–282.
7. Sclabas GM, Swain P, Swanstrom LL. Endoluminal methods for gastrotomy closure in natural orifice transenteric surgery (NOTES). Surg Innov. 2006. 13:23–30.
8. Pelosi MA, Pelosi MA 3rd. Laparoscopic appendectomy using a single umbilical puncture (minilaparoscopy). J Reprod Med. 1992. 37:588–594.
9. D'Alessio A, Piro E, Tadini B, Beretta F. One-trocar transumbilical laparoscopic-assisted appendectomy in children: our experience. Eur J Pediatr Surg. 2002. 12:24–27.
10. Ates O, Hakguder G, Olguner M, Akgur FM. Single-port laparoscopic appendectomy conducted intracorporeally with the aid of a transabdominal sling suture. J Pediatr Surg. 2007. 42:1071–1074.
11. Vidal O, Valentini M, Ginesta C, Marti J, Espert JJ, Benarroch G, et al. Laparoendoscopic single-site surgery appendectomy. Surg Endosc. 2010. 24:686–691.
12. Roberts KE. True single-port appendectomy: first experience with the "puppeteer technique". Surg Endosc. 2009. 23:1825–1830.
13. Kalloo AN, Singh VK, Jagannath SB, Niiyama H, Hill SL, Vaughn CA, et al. Flexible transgastric peritoneoscopy: a novel approach to diagnostic and therapeutic interventions in the peritoneal cavity. Gastrointest Endosc. 2004. 60:114–117.
14. Marescaux J, Dallemagne B, Perretta S, Wattiez A, Mutter D, Coumaros D. Surgery without scars: report of transluminal cholecystectomy in a human being. Arch Surg. 2007. 142:823–826.
15. Jagannath SB, Kantsevoy SV, Vaughn CA, Chung SS, Cotton PB, Gostout CJ, et al. Peroral transgastric endoscopic ligation of fallopian tubes with long-term survival in a porcine model. Gastrointest Endosc. 2005. 61:449–453.
16. Park PO, Bergstrom M, Ikeda K, Fritscher-Ravens A, Swain P. Experimental studies of transgastric gallbladder surgery: cholecystectomy and cholecystogastric anastomosis (videos). Gastrointest Endosc. 2005. 61:601–606.
17. Whiteford MH, Denk PM, Swanstrom LL. Feasibility of radical sigmoid colectomy performed as natural orifice translumenal endoscopic surgery (NOTES) using transanal endoscopic microsurgery. Surg Endosc. 2007. 21:1870–1874.
18. Lacy AM, Delgado S, Rojas OA, Almenara R, Blasi A, Llach J. MA-NOS radical sigmoidectomy: report of a transvaginal resection in the human. Surg Endosc. 2008. 22:1717–1723.
19. Leroy J, Cahill RA, Perretta S, Forgione A, Dallemagne B, Marescaux J. Natural orifice translumenal endoscopic surgery (NOTES) applied totally to sigmoidectomy: an original technique with survival in a porcine model. Surg Endosc. 2009. 23:24–30.
20. Hong TH, Kim HL, Lee YS, Kim JJ, Lee KH, You YK, et al. Transumbilical single-port laparoscopic appendectomy (TUSPLA): scarless intracorporeal appendectomy. J Laparoendosc Adv Surg Tech A. 2009. 19:75–78.
21. Feste JR, Bojahr B, Turner DJ. Randomized trial comparing a radially expandable needle system with cutting trocars. JSLS. 2000. 4:11–15.
22. Yim SF, Yuen PM. Randomized double-masked comparison of radially expanding access device and conventional cutting tip trocar in laparoscopy. Obstet Gynecol. 2001. 97:435–438.
23. Bhoyrul S, Payne J, Steffes B, Swanstrom L, Way LW. A randomized prospective study of radially expanding trocars in laparoscopic surgery. J Gastrointest Surg. 2000. 4:392–397.
24. Kaouk JH, Goel RK, Haber GP, Crouzet S, Desai MM, Gill IS. Single-port laparoscopic radical prostatectomy. Urology. 2008. 72:1190–1193.
25. Hong TH, You YK, Lee KH. Transumbilical single-port laparoscopic cholecystectomy: scarless cholecystectomy. Surg Endosc. 2009. 23:1393–1397.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download