Introduction
Inflammatory pseudotumor (IPT) is a clinical condition characterized by proliferation of spindle cells, inflammatory cells, and small vessels. IPT was first described in the lung,(1) but has also been reported in other anatomical sites, including the orbit, liver, spleen, and so on. Due to such a variety of anatomical sites, clinical manifestations can vary as well. We recently experienced a 65 year-old woman diagnosed with IPT of the lymph node in the splenic hilar, or distal supra-pancreatic area, mimicking gastric submucosal tumor. This lesion is extremely rare and has not been cited in the current literature. We describe such a rare case of IPT with a review of the literature.
CASE REPORT
A 65-year-old woman presented with gastric submucosal tumor incidentally detected by gastroscopy during physical examination. Otherwise, the patient was in good health, with no symptoms of unexplained fever, general ache, or weight loss. Findings from physical examination were unremarkable. The initial biochemical and hematologic investigation, including complete blood count, electrolytes, liver function tests, and chest radiograph were all within normal ranges.
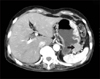
Gastroscopic examination showed a bulging mucosa, about 3×3 cm in diameter in the greater curvature side of the gastric body (Fig. 1A). Endoscopic ultrasound of the stomach showed a hypoechoic lesion in the muscularis propria layer, 2.5×2.0 cm in diameter, in the greater curvature side of the gastric body (Fig. 1B). Non-contrast and contrast abdominal computed tomography (CT) found a well-defined exophytic mass, with early enhancing nature in the greater curvature side of the gastric body (Fig. 2). Our results lead us to consider gastric submucosal tumor, including GIST, schawannoma, leiomyoma, and so on.
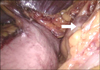
Surgical intervention was indicated, and laparoscopic exploration was performed thereafter. There was no specific abnormality in gastric wall. Therefore, there was no evidence of gastric submucosal tumor. The tumor was found during surgery in a location between the upper border of the distal pancreas and the splenic hilum (Fig. 3).
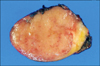
The tumor was removed without event using the laparoscopic method. Examination of frozen sections found lymph nodes with no evidence of malignancy. The lymph node in the specimen measured 3.3×3.0×2.2 cm and weighed 12.7 g (Fig. 4). Microscopically, the lymph node showed plasma cell infiltration and sclerosis in the focal area. The inflammatory cells infiltrate, including plasma cells, lymphocytes, eosinophils, and sclerosis were also noted in the perinodal soft tissues (Fig. 5). There was no evidence of malignancy. Features were consistent with a diagnosis of IPT of the lymph node.
The patient's postoperative course was uneventful, and she is doing well following surgery.
DISCUSSION
IPT is a clinical condition characterized by the appearance of inflammatory masses first described in the lung.(1) A number of alternative names have been used to refer to IPT, including inflammatory myofibroblastic tumor, plasma cell granuloma, or pseudotumor, xanthomatous pseudotumor, and so on. Although the cause and pathogenesis of IPT still remain controversial, it has been generally accepted that they may correspond with an unusual tissue response to injury.(2)
IPT has been reported in various anatomical sites, including the orbit, lung, liver, spleen, and so on. IPT of the lymph node is uncommon. IPT of the lymph node was first described in 1988.(3) Since then, few case reports or articles on IPT in the lymph node have been published. However, IPT of the lymph node in the splenic hilum or supra-pancreatic area is extremely rare, with no reports in the literature.
The clinical presentation of IPT varies greatly, depending on location. General symptoms (fever, fatigue, anorexia, weight loss, and sleeplessness) occur in 5~30% of IPT cases. Abnormal lymph node findings are mostly confined to one or two nodal areas.(4)
In the present case, clinical manifestation incidentally discovered gastric submucosal tumor with no other systemic manifestations.
According to Perrone et al.(3), there are two main patterns of IPT of the lymph nodes. The first group includes asymptomatic patients with localized lymphadenopathy and the second group comprised symptomatic patients with a number of laboratory abnormalities, such as elevated ESR, polyclonal hypergammaglobulinemia, mild anemia, elevated lactate dehydrogenase (LDH), and evidence of one or more enlarged lymph nodes. The clinical manifestation of the second group is similar to fever of unknown origin (FUO). Therefore, the problem of the second group is that differential diagnosis of FUO has to be made among a large number of clinical entities. Only histologic evidence can allow a correct diagnosis.(5)
In the radiologic report for IPT of the lymph node, contrast-enhanced CT of the neck demonstrated several lymph nodes with uniform low attenuation. The tumor did not demonstrate significant contrast enhancement.(6) Conversely, in the present case, the abdomen CT scan showed a well defined mass with enhancement.
Treatment of IPT generally involves the use of high dosages of corticosteroids. In the majority of cases, there is a dramatic effect showing diminished symptoms within 24~48 hours, and nearly complete resolution within 5~7 days. In the literature, however, no reports have been found on a recommended duration of therapy. In addition, response to several agents has been reported, including nonsteroidal anti-inflammatory agents,(7) chemotherapy and/or radiation therapy, and antibiotics.(8)
While IPT is benign, the outcome for patients with lesions can be a poor one, due to local infiltration, risk of recurrence, and variations in tumor aggressiveness. According to Kojima et al.,(8) relapse rate following treatment was reported at 15%. Therefore, some authors have proposed surgical excision as the therapy of choice whenever possible.(9) According to Andrade et al.,(10) surgical resection may be the treatment of choice in some cases when surgery can be performed simply for local decompression and relief of symptoms, with the exception of orbital lesions. In the present case, it was difficult to confirm a preoperative diagnosis. Therefore, surgical excision is inevitable when a correct preoperative diagnosis is impossible. We are of the opinion that laparoscopic excision is feasible in abdominal IPT if surgical excision is needed.
In conclusion, IPT of the lymph node in the splenic hilar or distal suprapancreatic area is extremely rare, and no reports have been cited in the literature. Its recognition is important, in order to avoid inadequate therapeutic measures, since it can clinically imitate gastric submucosal tumor.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download