Abstract
The differential diagnosis of mediastinal lymph node enlargement is mandatory, since the diagnosis of mediastinal lymph node enlargement covers a broad spectrum of diseases including inflammatory reactions, infections, and cancer metastases. We describe here a 51-year-old woman with anthracosis in mediastinal lymph node, mimicking metastatic carcinoma from the thyroid gland.
Since the term anthracosis was first used with reference to the lungs of coal workers in 1838, anthracosis is recognized to be related to the inhalation and deposition of carbon particles in the lungs and is classified as one of the pneumoconiosis.(1) It is also called black lung disease, black lung, black spittle, coal worker's pneumoconiosis, miner's asthma, pneumoconiosis, and silicosis. Lungs and mediastinal lymph nodes are usually affected by the carbon particles.(2)
Papillary thyroid carcinoma has a tendency to metastasize to regional lymph nodes, and the first step of nodal involvement is generally the central compartment lymph nodes, following by the lateral neck and the superior mediastinal nodes.(3)
The cause of mediastinal lymph node enlargement varies from the benign conditions such as inflammatory reactions and infections to the malignant conditions including primary mediastinum tumors and metastasis from other primary cancers. Thus, differential diagnosis of mediastinal lymph node enlargement is mandatory.
We describe here a female patient with anthracosis in mediastinal lymph node, which has mimicked metastatic lymph nodes from papillary thyroid carcinoma.
A 51-year-old woman presented with incidentally found thyroid nodule at medical check up. The patients had no constitutional symptoms, such as cough, shortness of breath, fever, fatigue, and weight loss, and no specific medical and occupational history. Cervical ultrasonography and computed tomography showed a 0.8-cm sized nodule in right thyroid gland, and fine-needle aspiration cytology was confirmed as a papillary thyroid carcinoma. A right hemithyroidectomy was performed, and histopathological examination confirmed papillary thyroid carcinoma.
Three years after the initial operation, lateral neck node metastases were detected in the routine follow up. A completion total thyroidectomy along with bilateral neck dissection was performed. Postoperative histopathological examinations revealed six metastatic nodes out of 106 removed nodes, but no lesions in the thyroid. The patient underwent postoperative high-dose (150 mCi) radioactive iodine treatment for ablation, and a post-treatment whole body scan showed no abnormal uptakes in the thyroid bed and other body areas.
One year after the second operation, the patient presented with palpable mass in the right supraclavicular space. Cervical ultrasonography and computed tomography demonstrated an enlarged mass with ill-defined margin in right supraclavicular fossa (Fig. 1). The preoperative histopathologic confirmation was not easy due to the location of the lesion. Serum thyroglobulin (levothyroxine-on) concentration was 0.6 ng/ml (normal, 0.1~32.5 ng/ml), and serum thyroglobulin-antibody concentration was <10.0 IU/ml (10~124.2 IU/ml). Other laboratory tests were within normal ranges.
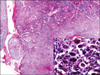
The mass was removed. Operative findings showed a 4.5 cm sized hard, fixed mass in right supraclavicular fossa, which was a unilocular cystic and abutting clavicle and subclavian vein. In addition, other multiple conglomerated enlarged lymph nodes, not detected in CT scans, were found in anterior superior mediastinum during the operation. For complete excision, anterior superior mediastinum lymph node dissection was added via sternotomy, and en bloc resection was performed. Histopathological examination of the mass turned out to be anthracosis combined with hemangioma or organizing hematoma, but there was no evidence of metastasis from papillary thyroid carcinoma (Fig. 2). There were any lung parenchymal changes such as small nodules or fibrotic change seen in pneumoconiosis on chest radiograph. The patient was discharged from the hospital 4 days after surgery, and three years after third surgery the patient remains free of disease.
Anthracosis is the asymptomatic accumulation of coal pigment without consequent cellular reaction. Inhaled coal dust causes a problem when the body's natural defense and processing of the dust becomes overwhelmed and subsequently over-reactive. Such accumulation can be found in urban dwellers as well as in tobacco smokers. In the present case, however, the patient was a house-wife, and had no smoking and occupational histories. Dwelling in the city was a sole, suspicious environmental factor. Air pollution is thought to be the cause of the anthracosis in our patient.
The pathologic effects of the inhalation of dust particulate can occur not only in the lung parenchyma but also along the lymphatic route of drainage. Lungs and mediastinum lymph nodes are known to be primary site for the localization of carbon particles.(2)
Papillary thyroid carcinoma has a strong tendency to metastasize to regional lymph nodes. The first echelon of nodal involvement in thyroid cancer is generally the central compartment lymph nodes and subsequently spread to the nodes of the lateral neck and the superior mediastinum.(3)
Surgical dissection of upper mediastinal metastatic lymph nodes through either cervical incision or sternotomy can be performed with low rate of peri-operative complications.(4) Thus, if mediastinal lymph node metastasis is discovered in thyroid cancer patients, mediastinal node dissection should be considered.
In the present case, the preoperative histopathologic confirmation of tumor was not easy due to the adhesion for previous surgery and the location of the lesion. Iodine-131 whole body scan was seemed to be helpful, but it was not popular in our country. Positron emission tomography (PET) scan was also seemed to be helpful in this condition, but it has been well known that thyroid cancer cells have the limitations in concentration of 18-FDG.(5) Laboratory findings were not usually helpful, and intraoperative frozen biopsy was not easy also.
In the operative findings including the characteristics of tumor and the severe adhesions with adjacent tissues, the lesion was seemed to be the typical metastatic mass. And then, we planned to perform the radical surgery including sternotomy and mediastinal dissection.
Most patients with anthracosis are usually asymptomatic, and only symptomatic treatments are usually given. No further treatment was performed for our patient also.
In conclusion, mediastinal lymph node enlargement can be caused by several benign and malignant conditions. However, mediastinum lymph node dissection should be considered if metastasis from papillary thyroid carcinoma is suspected by appropriate diagnostic procedures. Molecular imaging and localization methods using molecular markers will be helpful to the accurate diagnosis of mediastinum mass pre- or intra-operatively in the future.
Figures and Tables
References
1. Vakharia BM, Pietruk T, Calzada R. Anthracosis of the esophagus. Gastrointest Endosc. 1990. 36:615–617.
2. Varghese LR, Stanley MW, Wakely PE Jr, Lucido ML, Mallery S, Bardales RH. A case report of anthracosilicotic spindle-cell pseudotumor of mediastinal lymph node: cytologic diagnosis by endoscopic ultrasound-guided fine-needle aspiration. Diagn Cytopathol. 2005. 33:268–272.
3. Hamming JF, Roukema JA. Clark OH, Duh QY, Kebebew E, editors. Management of regional lymph nodes in papillary, follicular, and medullary thyroid cancer. Textbook of Endocrine Surgery. 2005. 2nd ed. Philadelphia: Elsevier Saunders;195–206.
4. Khoo ML, Freeman JL. Transcervical superior mediastinal lymphadenectomy in the management of papillary thyroid carcinoma. Head Neck. 2003. 25:10–14.
5. Sisson JC, Ackermann RJ, Meyer MA, Wahl RL. Uptake of 18-fluoro-2-deoxy-D-glucose by thyroid cancer: implications for diagnosis and therapy. J Clin Endocrinol Metab. 1993. 77:1090–1094.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download