Abstract
Actinomycosis is a rare infection caused by Actinomyces species, normal commensal inhabitants of the human bronchial and gastrointestinal tract. Infection occurs after preceding mucosal break-down by variable causes. A preoperative diagnosis is difficult because of its nonspecific clinical features, mimicking malignancy, tuberculosis or other inflammatory diseases. We report a case of abdominal actinomycosis presenting as an omental mass, which coexists with ascending colon cancer. Actinomycosis was diagnosed by histopathologic demonstration of sulfur granules in a specimen resected by laparoscopic exploration. Following surgery, the patient was treated with IV penicillin (20 million IU/day) for 3 weeks, and follow-up colonoscopy showed adenocarcinoma in the ascending colon. The patient underwent right hemicolectomy, then treated with intravenous penicillin for 4 weeks postoperatively and oral penicillin for 6 months. The patient has been free of recurrence for 6 months.
Actinomycosis is an infrequent chronic suppurative infection which usually manifests as fistulas and sinuses or a mass that simulates a pseudo-neoplastic formation.(1) The main causative agent of human actinomycosis is Actinomycosis israelii, a gram-positive, filamentous anaerobic to microaerophilic bacterium.(2) They are the members of the endogenous flora of mucous membranes seem to only cause pathological infection after preceding mucosal breakdown.(2-4) Abdominal actinomycosis is often difficult to diagnose before operation because of its infrequent and chronic disease progression without any characteristic clinical features that may mimic malignancy, tuberculosis or Crohn's disease. Diagnosis is based on histopathological demonstration of sulfur granules in the specimen.(1,2,5-7) We report an unusual case of abdominal actinomycosis presenting as omental mass adhering to peritoneum coexist with ascending colon cancer. A review of the previous literatures was also presented.
A 51-year-old male, presenting with intermittent left upper quadrant abdominal pain for 3 months, admitted to our hospital. He has no remarkable medical history except well regulated insulin-dependent diabetes and hypertension. The vital signs are all in normal range. On physical examination, there were tenderness and rebound tenderness in left upper quadrant of abdomen with ill defined relatively hard, and fixed 3 cm sized mass. The laboratory findings including tumor markers were within normal limits, except for an elevated C-reactive protein level (0~0.5 mg/dl) of 2.66 mg/dl. There was a lesion 3.3×2.0 cm in size, ill defined soft tissue density in the left-sided omentum with enhancement and a 1.7 cm internal linear high density in abdomino-pelvic computed tomography (Fig. 1A). Mild adjacent fat infiltration and peritoneal thickening were noted, and foreign body with granulation tissue was considered. Ultrasonography (US) of abdomen also showed about 3.0×2.0 cm infiltrative ill defined hypoechoic lesion in the abdominal wall and omentum with suggestive foreign body reaction or malignancy, less likely (Fig. 1B). Because a malignancy was not completely ruled out, the patient underwent laparoscopic partial omentectomy (Fig. 2).
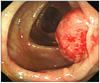
The histopathological findings were chronic inflammation and fibrosis with sulfur granule, composed of radiating filamentous bacteria, which is corresponding to the diagnosis of actinomycosis (Fig. 3). Following surgery, the patient was treated with intravenous penicillin injection (20 million IU/day) for 3 weeks, and colonoscopy which was done for follow-up showed a 2 cm sized tumor in right colon (Fig. 4). Under the diagnosis of adenocarcinoma of the ascending colon, the patient underwent right hemicolectomy. And the final histopathological evaluation showed adenocarcinoma, moderately differentiated, 2.2×1.8 cm in size at the ascending colon extension into submucosa and no metastasis in 11 harvested lymph nodes, stage I (AJCC TNM Staging System for colorectal cancer). Intraoperatively, no tumor was seen the other omentum and abdominal organs except ascending colon cancer mass. The patient was treated with intravenous penicillin (20 million IU/day) for 4 weeks postoperatively and oral penicillin (2 g/day) for 6 months. One month after surgery, he was nearly completely free of symptoms except mild intermittent perumbilical pain.
Actinomycosis is a rare and insidious clinical entity caused by the Actinomyces species, most commonly generated by Actinomycosis israelii, but rarely Arachnia propionica and Actinomyces naeslundii.(6) Actinomyces bacteria are considered to be saprophytes in the oral cavity, throughout gastrointestinal tract and female genital tract.(8) Depending on the site of primary infection, it is generally classified as cervicofacial (50%), abdominal (20%) and thoracic (15%) type.(1,5)
The breakdown of the mucosal barrier by trauma (previous surgery, endoscopic manipulation or bowel perforation etc.), immunosuppression (steroid therapy, diabetes mellitus or neoplasm), or chronic inflammatory disease caused by foreign body such as intrauterine contraceptive device, are recognized as predisposing factors for abdominal actinomycosis by penetration of the Actinomyces bacteria.(1,2,4-6,8,9)
Clinically, majority of the patients present nonspecific symptoms like abdominal pain and cramps, fever, anorexia, fatigue, weight loss, constipation or diarrhea which lasts for several months before being diagnosed, but there is no evidence of specific symptoms related to abdominal actinomycosis. The physical findings include a palpable mass. In laboratory analyses the dominating findings are anemia, leukocytosis and positive inflammation markers.(1,5-9)
The chronic granulomatous reaction with abscess formation in the peritoneal cavity causes mass lesions and luminal narrowing by extensive fibrosis and thickening in the bowel wall. Therefore, this clinical presentation simulate malignancy, intestinal tuberculosis and chronic appendicitis or inflammatory bowel diseases like Crohn's disease.(2,3,5-7,9)
In our case, the patient had clinical symptoms including abdominal pain for 3 months with the palpable mass and mild elevated acute phase reactant. He had no predisposing factors except the diabetes mellitus and ascending colon cancer that could cause actinomycosis.
The destruction of the mucosal barrier by immune suppression due to the diabetes mellitus could be the infection source of Actinomyces bacteria.(2,4-6) The location between the lesion of colon cancer and actinomycosis was too far to plausibly consider any relation between two diseases in our case. So far, there have been no clinical trials for reveal the relationship between these two diseases. But, the mucosal integrity of intestinal tract could be broken by cancerous lesion itself, we could not completely exclude the cancer a cause of actinomycosis. So, we recommended that endoscopic examination should be performed in actinomycosis patients for ruled out hidden malignancy.
Radiological studies can be used, but never as a conclusive diagnostic tool for actinomycosis.(1,2,4-6,8,9) In our case, computed tomography showed infiltrative solid mass with dense, non-homogeneous contrast enhancement mimicking malignancy. Ultrasonography also showed ill defined infiltrative hypoechoic lesion and sustained the suspicion on inflammatory change with foreign body reaction, rather than the malignancy.
In our patient, clinical presentation was nonspecific and preoperative hematologic and radiologic findings were not compatible with any specific diagnosis. We considered intestinal lymphoma, tuberculosis, foreign body reaction or malignancy in the differential diagnosis before laparoscopic exploration. The diagnosis is made preoperatively in less than 10% of patients because of the low index of suspicion, unusual presentation, and difficulty in culturing Actinomyces.(2)
The diagnosis is mostly made by histopathologic finding of typical sulfur granules and confirmed by microbiological culture of causative Actinomyces species.(1,2,5-7) Actinomyces granules show positive reaction with periodic acids stain consistently, we could diagnose actinomycosis in our patient.
Combined surgical excision of necrotic and infected tissue with long term antibiotic treatment has already been outlined as the most efficient, but so far, there have been no comparative trials comparing with the antibiotic treatment only for abdominal actinomycosis. Actinomyces israelii, the most common Actinomyces species is susceptible to penicillin G and tetracycline, which the treatment of choice. Initial treatment should be application of high dose intravenous penicillin G at 20 million IU/day for 4 weeks, followed by oral penicillin at a dose of 2~4 g/day for at least 6~12 months.(1-3,5,6,8,9)
In our case, the radical operation was done for the ascending colon cancer detected from colonoscopic examination which was done for follow-up study after 3 weeks after the diagnosis of actinomycosis. After the radical cancer surgery, he applied oral penicillin after weekly intravenous penicillin injection for 4 weeks, the clinical symptoms including the palpable mass and the abdominal pain disappeared with a normal range of inflammation markers.
In conclusion, abdominal actinomycosis should be considered in the differential diagnosis of patients who have symptoms such as a palpable mass and leukocytosis with predisposing factors for actinomycosis. In addition, we recommend the colonoscopic examination after diagnosis of actinomycosis for ruled out hidden malignancy.
Figures and Tables
Fig. 1
(A) Abdomino-pelvic computed tomography shows 3.3×2 cm ill defined soft tissue density in left-sided omentum with enhancement and 1.7 cm internal linear high density (white arrow). (B) Abdominal ultrasonography shows about 3 cm infiltrative ill defined hypoechoic lesion in left abdominal wall and omentum (white arrows).

Fig. 2
(A) Omental abscess resected by laparoscopic approach. (B) Intraoperative finding shows multiple small abscess formations located through omentum.

References
1. Joo YT. Abdominal actinomycosis presented as a periappendiceal abscess. J Korean Surg Soc. 2004. 67:342–345.
2. Kaya M, Sakarya MH. A rare cause of chronic abdominal pain, weight loss and anemia: abdominal actinomycosis. Turk J Gastroenterol. 2007. 18:254–257.
3. Filippou D, Psimitis I, Zizi D, Rizos S. A rare case of ascending colon actinomycosis mimicking cancer. BMC Gastroenterol. 2005. 5:1.
4. Hefny AF, Joshi S, Saadeldin YA, Fadlalla H, Abu-Zidan FM. Primary anterior abdominal wall actinomycosis. Singapore Med J. 2006. 47:419–421.
5. Kim SY, Lee HS, Kim SM, Lee WJ, Lee JY, Choi SJ, et al. A case of abdominal actinomycosis presenting as mesenteric mass. Korean J Gastroenterol. 2008. 51:48–51.
6. Lee SG, Roh YH, Park KJ, Choi HJ, Jung GJ, Han MS. The clinical study of abdominopelvic actinomycosis. J Korean Surg Soc. 2006. 70:47–52.
7. Jung EY, Choi SN, Park DJ, You JJ, Kim HJ, Chang SH. Abdominal actinomycosis associated with a sigmoid colon perforation in a patient with a ventriculoperitoneal shunt. Yonsei Med J. 2006. 47:583–586.
8. Filipovic B, Milinic N, Nikolic G, Ranthelovic T. Primary actinomycosis of the anterior abdominal wall: case report and review of the literature. J Gastroenterol Hepatol. 2005. 20:517–520.
9. Karagulle E, Turan H, Turk E, Kiyici H, Yildirim E, Moray G. Abdominal actinomycosis mimicking acute appendicitis. Can J Surg. 2008. 51:E109–E110.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download