Abstract
We report a case in which an intramural and intraluminal hematoma of the jejunum served as the lead point of intussusception in a 77-year-old man with warfarinization. The patient presented with cramping abdominal pain and vomiting. Palpation of the abdomen revealed periumbilical tenderness. Abdominal computed tomography revealed a circular mass with a concentric ring, consistent with an intussuscepted jejunum. Because of warfarinization, which was due to atrial fibrillation and lacunar infarction, the patient's prothrombin time was prolonged. Laparotomy revealed reducible jejuno-jejunal intussusception, and we performed a segmental resection of the intussuscepted jejunum. We identified an intramural and intraluminal jejunal hematoma as the lead point. Upon histopathological examination, angiodysplasia of the intussuscepted jejunum was found to be the bleeding focus. No similar case was found in the literature.
Warfarin is an oral anticoagulant that has been used for more than 50 years to treat and manage various diseases, such as pulmonary embolism, deep vein thrombosis, prosthetic valves, and persistent atrial fibrillation.(1,2) However, despite its widespread use and efficacy, there have been a number of problems associated with warfarin use. These problems have included the need for monitoring the prothrombin time (PT), its narrow therapeutic index, and especially the risk of bleeding. Bleeding is the major complication of warfarin use and may threaten the patient's life with intracranial and pericardial hemorrhage or massive gastrointestinal blood loss. Intestinal intramural and intraluminal hematoma is a rare complication of warfarin.(3)
We describe a spontaneous intestinal intramural and intraluminal hematoma as the lead point of jejuno-jejunal intussusception caused by warfarin overdose in a nontrauma patient. Adult jejuno-jejunal intussusception is also a rare entity. It is quite rare for an intramural and intraluminal hematoma to serve as the lead point. To the best of our knowledge, there are two reported cases of intussusception caused by intramural hematoma in patients with hemophilia, and this is the first reported case of jejuno-jejunal intussusception caused by intramural and intraluminal hematoma in a patient with warfarinization.
A 77-year-old Korean man was brought to the emergency room with complaints of cramping abdominal pain and vomiting. The patient had been admitted to the Neurology Department of our hospital 3 years prior because of lacunar infarction and atrial fibrillation. Since that time, the patient was treated with 4 mg warfarin as an outpatient. One month prior to the emergency visit, the patient had been admitted to the Gastrointestinal Department because of duodenal ulcer bleeding.
On admission, the patient was afebrile with a blood pressure of 180/90 mmHg and a pulse of 68 beats/min. Pale sclera or melena was not noted. There was no evidence of bleeding. Abdominal examination revealed a rigid, non-distended abdomen with epigastric tenderness but without rebound tenderness. No masses or contusions were noted. Bowel sounds were nearly normoactive. The results of the neurological examinations were within normal limits.
Laboratory data on admission were as follows: white blood count 7,200/cu mm, hemoglobin 10.1 g/dl, hematocrit 32.0%, platelet count 188,000/mm3, PT 10.1% (INR 4.52), partial thromboplastin time 55.5 sec, amylase 135 U/L (normal 28~110), and electrolytes were within normal limits. Urinalysis revealed occult hematuria.
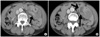
Plain chest and simple abdomen X-ray were normal and an abdomen-pelvic computed tomography (CT) with enhancement was performed. The CT revealed focal proximal jejunal dilatation due to jejuno-jejunal intussusception with wall thickening (Fig. 1).
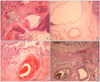
Emergency laparotomy was performed. The jejunum approximately 30 cm distal from Treitz's ligament was intussuscepted along a 30 cm length. After a successful attempt at Hutchinson's maneuver, the intussuscepted jejunum was discolored dark brown and had no motility. We performed a segmental resection and anastomosis. The resected bowel was filled with a hematoma that was fixed to the mucosa (Fig. 2). Histopathological examination revealed angiodysplasia in the bleeding focus (Fig. 3).
The patient had an uneventful postoperative recovery and was discharged from the hospital and followed up in our outpatient clinic.
Anticoagulant is used to treat a wide range of cardiac, pulmonary, vascular, and neurological diseases. Although more specific new generation anticoagulant drugs are becoming increasingly popular, warfarin is still most widely used oral anticoagulant worldwide.(1,2) Among patients treated with warfarin, there is little correlation between dose, serum concentration, and therapeutic effect so it is necessary to regulate the dosage individually, guided by INR monitoring. Excessive anticoagulation and bleeding are the most common complication of warfarin therapy.(4) In the present case, the patient had taken 4 mg warfarin daily and the INR was 4.52 in the emergency room.
Approximately 100 cases of intramural hematoma of the small intestine associated with anticoagulant therapy have been reported in the literature.(5) The most common sites for intramural hematoma of the small intestine are the duodenum and proximal jejunum. A sudden increase in intra-abdominal pressure has been postulated to cause a stretching and retraction of the bowel wall capable of producing tears in the submucosal blood vessels.(6) However, the exact pathogenesis of the intramural hematoma associated with anticoagulant therapy is not known. In the present case, the bleeding focus was the angiodysplasia of the jejunum. The intraluminal hematoma was hardly fixed to the mucosa at the focus of bleeding and served as the lead point of the intussusception.
To the best of our knowledge, the present case, in which an intramural and intraluminal hematoma of the jejunum developed and became the lead point of intussusception in an elderly patient with warfarinization, is the first such case. The first intussusception that was associated with a bleeding tendency was reported in 1904,(7) and it was intestinal intussusception that was associated with Henoch's purpura. Intussusception due to submucosal hematoma is not uncommonly seen in children with anaphylactoid purpura,(8) and there are several reports of intussusception in hemophilia patients.(8-10)
Figures and Tables
References
1. Hirsh J. Oral anticoagulant drugs. N Engl J Med. 1991. 324:1865–1875.
2. Shah P, Kraklow W, Lamb G. Unusual complication of coumadin toxicity. Wis Med J. 1994. 93:212–214.
3. Majerus PW, Broze GJ, Miletich JP, Tollefsen DM. Gilman GG, Limbird L, Molinoff PB, Ruddon RW, Gilman A, editors. Anticoagulant, thrombolytic and antiplatelet drugs. Goodman & Gilman's: The Pharmacological Basis of Therapeutics. 1996. 9th ed. New York: McGraw-Hill;1341–1351.
4. Reynolds MW, Fahrbach K, Hauch O, Wygant G, Estok R, Cella C, et al. Warfarin anticoagulation and outcomes in patients with atrial fibrillation: a systematic review and metaanalysis. Chest. 2004. 126:1938–1945.
5. Hughes CE 3rd, Conn J Jr, Sherman JO. Intramural hematoma of the gastrointestinal tract. Am J Surg. 1977. 133:276–279.
6. Devroede GJ, Tirol FT, Lo Russo VA, Narducci AE. Intramural hematoma of the duodenum and jejunum. Am J Surg. 1966. 112:947–954.
7. Sutherland GA. Intussusception and Henoch's purpura. Br J Dis Child. 1904. 1:23–28.
8. Collins DL, Miller KE. Intussusception in hemophilia. J Pediatr Surg. 1968. 3:599–603.
9. LeBlanc KE. Jejuno-jejunal intussusception in a hemophiliac: a case report. Ann Emerg Med. 1982. 11:149–151.
10. Nakayama Y, Fukushima M, Sakai M, Hisano T, Nagata N, Shirahata A, et al. Intramural hematoma of the cecum as the lead point of intussusception in an elderly patient with hemophilia A: report of a case. Surg Today. 2006. 36:563–565.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download