Abstract
Purpose
This study was performed to evaluate the feasibility of the Gamma Knife Surgery on the symptomatic control of brain metastasis from breast carcinoma.
Methods
We retrospectively reviewed patients with brain metastases from breast cancer who underwent Gamma Knife Surgery at our hospital, between May 2004 and November 2007. Total 82 metastases were treated with 26 cycles of Leksell gamma knife. Freedom from local recurrence and survival time were analyzed by the Kaplan-Meier method.
Results
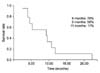
17 patients with 82 metastases were treated over 26 Gamma Knife Surgery sessions. The mean time to brain metastases was 41.7 months (8~84), median number was 2.0 (1~10), and median volume was 7.4 cm3 (0.6~25.4). Radiologic response occurred in 84.6%, and the rate of symptom relief was 73.1%. Local brain tumor recurrences were observed in 15.3% and intracranial distant recurrence occurred in 57.7% that occurred within 3.2 months. The median length of survival for all patients was 9.3 months (95% confidence interval, 4.23~9.37 months).
References
1. Kamby C. The pattern of metastases in human breast cancer: methodological aspects and influence of prognostic factors. Cancer Treat Rev. 1990. 17:37–61.
2. Tsukada Y, Fouad A, Pickren JW, Lane WW. Central nervous system metastasis from breast carcinoma. Autopsy study. Cancer. 1983. 52:2349–2354.
3. Posner JB. Neurologic Complications of Cancer. 1995. Philadelphia: F.A.Davis;96.
4. Gaspar LE, Scott C, Murray K, Curran W. Validation of the RTOG recursive partitioning analysis (RPA) classification for brain metastases. Int J Radiat Oncol Biol Phys. 2000. 47:1001–1006.
5. Mahmoud-Ahmed AS, Suh JH, Lee SY, Crownover RL, Barnett GH. Results of whole brain radiotherapy in patients with brain metastases from breast cancer: a retrospective study. Int J Radiat Oncol Biol Phys. 2002. 54:810–817.
6. Chang EL, Lo S. Diagnosis and management of central nervous system metastases from breast cancer. Oncologist. 2003. 8:398–410.
7. Wen PY, Loeffler JS. Management of brain metastases. Oncology (Williston Park). 1999. 13:941–954.
8. Wronski M, Arbit E, McCormick B. Surgical treatment of 70 patients with brain metastases from breast carcinoma. Cancer. 1997. 80:1746–1754.
9. Pieper DR, Hess KR, Sawaya RE. Role of surgery in the treatment of brain metastases in patients with breast cancer. Ann Surg Oncol. 1997. 4:481–490.
10. Rosner D, Nemoto T, Lane WW. Chemotherapy induces regression of brain metastases in breast carcinoma. Cancer. 1986. 58:832–839.
11. Adler JR, Cox RS, Kaplan I, Martin DP. Stereotactic radiosurgical treatment of brain metastases. J Neurosurg. 1992. 76:444–449.
12. Mehta MP, Rozental JM, Levin AB, Mackie TR, Kubsad SS, Gehring MA, et al. Defining the role of radiosurgery in the management of brain metastases. Int J Radiat Oncol Biol Phys. 1992. 24:619–625.
13. Alexander E 3rd, Moriarty TM, Davis RB, Wen PY, Fine HA, Black PM, et al. Stereotactic radiosurgery for the definitive, noninvasive treatment of brain metastases. J Natl Cancer Inst. 1995. 87:34–40.
14. Caron JL, Souhami L, Podgorsak EB. Dynamic stereotactic radiosurgery in the palliative treatment of cerebral metastatic tumors. J Neurooncol. 1992. 12:173–179.
15. Coffey RJ, Flickinger JC, Bissonette DJ, Lunsford LD. Radiosurgery for solitary brain metastases using the cobalt-60 gamma unit: methods and results in 24 patients. Int J Radiat Oncol Biol Phys. 1991. 20:1287–1295.
16. Flickinger JC, Kondziolka D, Lunsford LD, Coffey RJ, Goodman ML, Shaw EG, et al. A multi-institutional experience with stereotactic radiosurgery for solitary brain metastasis. Int J Radiat Oncol Biol Phys. 1994. 28:797–802.
17. Kihlstrom L, Karlsson B, Lindquist C. Gamma Knife surgery for cerebral metastases. Implications for survival based on 16 years experience. Stereotact Funct Neurosurg. 1993. 61:Suppl 1. 45–50.
18. Firlik KS, Kondziolka D, Flickinger JC, Lunsford LD. Stereotactic radiosurgery for brain metastases from breast cancer. Ann Surg Oncol. 2000. 7:333–338.
19. Bindal AK, Bindal RK, Hess KR, Shiu A, Hassenbusch SJ, Shi WM, et al. Surgery versus radiosurgery in the treatment of brain metastasis. J Neurosurg. 1996. 84:748–754.
20. Joseph J, Adler JR, Cox RS, Hancock SL. Linear accelerator-based stereotaxic radiosurgery for brain metastases:the influence of number of lesions on survival. J Clin Oncol. 1996. 14:1085–1092.
21. Varlotto JM, Flickinger JC, Niranjan A, Bhatnagar AK, Kondziolka D, Lunsford LD. Analysis of tumor control and toxicity in patients who have survived at least one year after radiosurgery for brain metastases. Int J Radiat Oncol Biol Phys. 2003. 57:452–464.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download