1. Peter NG, Clark LR, Jaeger JR. Fitz-Hugh-Curtis syndrome: a diagnosis to consider in women with right upper quadrant pain. Cleve Clin J Med. 2004. 71:233–239.
2. Fitz-Hugh T Jr. Acute gonococcic peritonitis of the right upper quadrant in women. JAMA. 1934. 102:2094–2096.
3. Curtis AH. A cause of adhesions in the right upper quadrant. JAMA. 1930. 94:1221–1222.
4. Muller-Schoop JW, Wang SP, Munzinger J, Schlapfer HU, Knoblauch M, Tammann RW. Chlamydia trachomatis as possible cause of peritonitis and perihepatitis in young women. Br Med J. 1978. 1:1022–1024.
5. Wang SP, Eschenbach DA, Holmes KK, Wager G, Grayston JT. Chlamydia trachomatis infection in Fitz-Hugh-Curtis syndrome. Am J Obstet Gynecol. 1980. 138:1034–1038.
6. Lopes-Zeno JA, Keith LG, Berger GS. The Fitz-Hugh-Curtis syndrome revisited: changing perspectives after half a century. J Reprod Med. 1985. 30:567–582.
7. Sharma JB, Roy KK, Gupta N, Jain SK, Malhotra N, Mittal S. High prevalence of Fitz-Hugh-Curtis syndrome in genital tuberculosis. Int J Gynecol Obstet. 2007. 99:62–63.
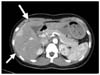
8. Nishie A, Yoshimiusu K, Irie H, Yoshitake T, Aibe H, Tajima T, et al. Fitz-Hugh-Curtis syndrome radiologic manifestation. J Comput Assist Tomogr. 2003. 27:786–791.
9. Oh JH, Cho YS, Choi YH, Lee HS. A diagnostic utility of Fitz-Hugh-Curtis syndrome by using contrast enhanced abdominopelvic computerized tomography. J Korean Soc Emerg Med. 2005. 16:410–415.
10. Jin SC, Sohn YD, Choi WI. Two cases of Fitz-Hugh-Curtis syndrome diagnosed by abdominopelvic computerized tomography. Keimyung Med J. 2006. 26:52–56.
11. Lee SC, Nah BG, Kim HS, Choi TH, Lee SH, Lee JY, et al. Two cases of Fitz-Hugh-Curtis syndrome in acute phase. Korean J Gastroenterol. 2005. 45:137–142.
12. Zeger W, Holt K. Gynecologic infections. Emerg Med Clin North Am. 2003. 21:631–648.
13. Tsubuku M, Hayashi S, Terahara A, Furukawa T, Ohmura G. Fitz-Hugh-Curtis syndrome: linear contrast enhancement of the surface of the liver on CT. J Comput Assist Tomogr. 2002. 26:456–458.
14. Kechagia N, Bersimis S, Chatzipanagiotou S. Incidence and antimicrobial susceptibilities of genital mycoplasmas in outpatient women with clinical vaginitis in Athens, Greece. J Antimicrob Chemother. 2008. 62:122–125.
15. McCormick M, DelCastillo J, Berk RS. An atypical presentation of the Fitz-Hugh-Curtis syndrome. J Emerg Med. 1990. 8:55–58.






 PDF
PDF ePub
ePub Citation
Citation Print
Print








 XML Download
XML Download