Abstract
Purpose
To report a case of moyamoya syndrome after an additional diagnosis of neurofibromatosis type 1 (NF 1) using an ophthalmic examination in a middle-aged patient with moyamoya disease.
Case summary
A 60-year-old male with no specific past medical history except moyamoya disease visited our hospital for an ophthalmic examination. Two years prior, he had been diagnosed with moyamoya disease by brain imaging performed after a head trauma. At the first visit, his best corrected visual acuity was no light perception in the right eye (OD) and 20/25 in the left eye (OS). The intraocular pressure was 8 mmHg (OD) and 10 mmHg (OS). On fundus examination, the right eye showed a dense opacity of an ocular media and the left eye showed no abnormality except an increased cup-to-disc ratio. However, infrared imaging showed multiple whitish lesions in the left eye. Fluorescein angiography showed a patchy choroidal filling delay. During the follow-up, slit-lamp microscopy revealed Lisch nodules and multiple café au lait spots and neurofibromas were found in the skin which led to the diagnosis of NF 1.
Conclusions
When examining patients with moyamoya disease, ophthalmologists should check not only ocular comorbidity associated with moyamoya disease but also ocular comorbidity with other systemic diseases that can accompany moyamoya disease. NF 1 is the most common systemic disease associated with moyamoya syndrome. In this case, appropriate follow-up was essential to monitor the development of ocular or systemic vasculopathies and their complications.
Figures and Tables
Figure 1
Brain computed tomography (CT) (A–C), and transfemoral cerebral angiography (TFCA) (D, E). (A) CT scan shows subarachnoid hemorrhage in anterior flax (white arrow). (B) Non-contrast enhanced CT scan at the level of thalamus and occipital lobe shows no abnormality in the bilateral visual pathway. (C) Contrast-enhanced CT scan shows neither mass nor enhancing lesion around bilateral optic nerves. Note the calcification of right eye (white arrow). (D, E) Right and left internal carotid artery (ICA) and its branches, respectively. TFCA shows narrowing of right ICA (white arrow) and middle cerebral artery (MCA) (white arrowhead) compared to left ICA and MCA.
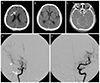
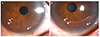
Figure 2
Color fundus photo, peripapillary circular optical coherent tomography (OCT) scan, fluorescein angiography, infrared fundus image, and retinal OCT scan of the left eye. (A) Color fundus photo shows normal fundus findings except increased cup-disc ratio. (B) Peripapillary circular OCT scan shows decreased peripapillary retinal nerve fiber layer thickness. (C) Fluorescein angiography shows multiple delayed, patchy choroidal filling, which means that there is a problem in choroidal circulation. (D) Infrared fundus image shows multiple whitish lesions in the posterior pole. (E) OCT scan shows that one of these whitish lesions (white arrow in D) is located in the choroid with hyperreflectivity (white arrow in E). These lesions are called choroidal nodules and are frequently seen in patients with neurofibromatosis type 1.1314

Notes
References
2. Williams M, Adas A, Sharma N, Gibson M. Moyamoya disease presenting to the ophthalmology clinic. Can J Ophthalmol. 2006; 41:633–634.

3. Phi JH, Wang KC, Lee JY, Kim SK. Moyamoya syndrome: a window of moyamoya disease. J Korean Neurosurg Soc. 2015; 57:408–414.

4. Huson S, Jones D, Beck L. Ophthalmic manifestations of neurofibromatosis. Br J Ophthalmol. 1987; 71:235–238.

5. Bang J, Yang HS, Ahn JH, et al. Ophthalmic manifestations in patients with neurofibromatosis. J Korean Ophthalmol Soc. 2008; 49:1829–1838.

6. Takeuchi K, Shimizu K. Hypoplasia of the bilateral internal carotid arteries. Brain Nerve. 1957; 9:37–43.
7. Suzuki J, Takaku A. Cerebrovascular “moyamoya” disease. Disease showing abnormal net-like vessels in base of brain. Arch Neurol. 1969; 20:288–299.
8. Witmer MT, Levy R, Yohay K, Kiss S. Ophthalmic artery ischemic syndrome associated with neurofibromatosis and moyamoya syndrome. JAMA Ophthalmol. 2013; 131:538–539.

9. Ferner RE. Neurofibromatosis 1 and neurofibromatosis 2: a twenty first century perspective. Lancet Neurol. 2007; 6:340–351.

10. Lee YH, Kim KN, Shin KS, Kim JY. Hemi-central retinal vein occlusion in a patient with neurofibromatosis 1. J Korean Ophthalmol Soc. 2010; 51:150–154.

12. Hamilton SJ, Freidman JM. Insights into the pathogenesis of neurofibromatosis 1 vasculopathy. Clin Genet. 2000; 58:341–344.

13. Viola F, Villani E, Natacci F, et al. Choroidal abnormalities detected by near-infrared reflectance imaging as a new diagnostic criterion for neurofibromatosis 1. Ophthalmology. 2012; 119:369–375.

14. Abdolrahimzadeh S, Felli L, Plateroti R, et al. Morphologic and vasculature features of the choroid and associated choroid-retinal thickness alterations in neurofibromatosis type 1. Br J Ophthalmol. 2015; 99:789–793.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download