Abstract
Purpose
To investigate the surgical results of early silicone tube displacement in congenital nasolacrimal duct obstruction.
Methods
A total of 40 eyes from 27 children who received silicone tube intubation with sequential probing under intranasal endoscopic guidance were enrolled in this retrospective study. The silicone tube was intended to be removed after 3 months, and was defined as early displacement if the tube was removed within 2/3 of the planned tube retention time. Success was defined as the absence of persistent epiphora for at least a 1-year follow-up period. Using Fisher's exact test, the success rate of patients with and without early tube displacement was compared for a statistical difference.
Results
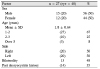
Overall, 95% (38/40) of eyes were treated successfully; they were not affected by early tube displacement (p=0.154). Early displacement occurred in 40% (16/40) of eyes: 12% (2) within 7 days, 44% (7) within 8–14 days, 19% (3) within 15–30 days, and 25% (4) after 31 days.
Conclusions
In congenital nasolacrimal duct obstruction, early silicone tube displacement did not affect the clinical outcome of silicone tube intubation. Therefore, endoscopic-guided silicone tube intubation with sequential probing may provide a high functional success rate although early tube displacement occurs in young children.
Figures and Tables
References
1. Noda S, Hayasaka S, Setogawa T. Congenital nasolacrimal duct obstruction in Japanese infants: its incidence and treatment with massage. J Pediatr Ophthalmol Strabismus. 1991; 28:20–22.
2. Paul TO, Shepherd R. Congenital nasolacrimal duct obstruction: natural history and the timing of optimal intervention. J Pediatr Ophthalmol Strabismus. 1994; 31:362–367.

3. Guerry D 3rd, Kendig EL Jr. Congenital impatency of the nasolacrimal duct. Arch Ophthal. 1948; 39:193–204.

4. Lee SY, Chung HS, Kim HB, et al. The incidence of congenital nasolacrimal duct obstruction in Korean neonates. J Korean Ophthalmol Soc. 1989; 30:5–8.
5. Oh HS, Ahn Y. The incidence and medical treatment of congenital nasolacrimal duct obstruction in Korean infants. J Korean Ophthalmol Soc. 1995; 36:1007–1013.
6. Paul TO. Medical management of congenital nasolacrimal duct obstruction. J Pediatr Ophthalmol Strabismus. 1985; 22:68–70.

7. Petersen RA, Robb RM. The natural course of congenital obstruction of the nasolacrimal duct. J Pediatr Ophthalmol Strabismus. 1978; 15:246–250.

8. Welsh MG, Katowitz JA. Timing of silastic tubing removal after intubation for congenital nasolacrimal duct obstruction. Ophthal Plast Reconstr Surg. 1989; 5:43–48.

9. Park J, Lee YJ, Kim SJ, Jang JW. Factors affecting the outcome of silicone intubation for congenital nasolacrimal duct obstruction. J Korean Ophthalmol Soc. 2011; 52:266–271.

10. Pediatric Eye, Repka MX, Melia BM, et al. Primary treatment of nasolacrimal duct obstruction with nasolacrimal duct intubation in children younger than 4 years of age. J AAPOS. 2008; 12:445–450.
11. Peterson NJ, Weaver RG, Yeatts RP. Effect of short-duration silicone intubation in congenital nasolacrimal duct obstruction. Ophthal Plast Reconstr Surg. 2008; 24:167–171.

12. Katowitz JA, Welsh MG. Timing of initial probing and irrigation in congenital nasolacrimal duct obstruction. Ophthalmology. 1987; 94:698–705.

13. Mannor GE, Rose GE, Frimpong-Ansah K, Ezra E. Factors affecting the success of nasolacrimal duct probing for congenital nasolacrimal duct obstruction. Am J Ophthalmol. 1999; 127:616–617.

14. Dortzbach RK, France TD, Kushner BJ, Gonnering RS. Silicone intubation for obstruction of the nasolacrimal duct in children. Am J Ophthalmol. 1982; 94:585–590.

15. Durso F, Hand SI Jr, Ellis FD, Helveston EM. Silicone intubation in children with nasolacrimal obstruction. J Pediatr Ophthalmol Strabismus. 1980; 17:389–393.

16. Lee JJ, Ahn JH, Kim JL, Yang JW. The clinical outcome of endoscopic silicone tube intubation for congenital nasolacrimal duct obstruction. J Korean Ophthalmol Soc. 2012; 53:929–933.

17. Clark RA. Dilation probing as primary treatment for congenital nasolacrimal duct obstruction. J AAPOS. 2002; 6:364–367.

18. Youm JH, Lee H, Jang MW, et al. Monocanalicular and bicanalicular intubation with sequential probing for congenital nasolacrimal duct obstruction in patients over the age of 24 months. J Korean Ophthalmol Soc. 2013; 54:1635–1640.

19. Yoon TJ, Na KS, Yoon WJ. The effect of silicone tube intubation in pediatric nasolacrimal duct obstruction. J Korean Ophthalmol Soc. 2002; 43:155–159.
20. Cho KW, Lee SY, Kim SJ. Treatment of congenital nasolacrimal duct obstruction using silicone intubation set. J Korean Ophthalmol Soc. 1995; 36:553–558.
21. Leone CR Jr, Van Gemert JV. The success rate of silicone intubation in congenital lacrimal obstruction. Ophthalmic Surg. 1990; 21:90–92.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download