Abstract
Purpose
Methods
Results
Figures and Tables
Figure 1
Preoperative optical coherence tomography images of combined hamartoma of the retina and retinal pigment epithelium. These images showed the epiretinal membrane of combined hamartoma of the retina and retinal pigment epithelium and distorted fovea contour.
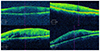
Figure 2
Epiretinal membrane (ERM) of combined hamartoma of the retina and retinal pigment epithelium in 73 years old man. (A) Preoperative fundus photo showed gray elevated lesion with preretinal gliosis, vascular tortuosity with vascular traction, hyperplasia of retinal pigment epithelium at the margin of growth. Preoperative visual acuity was logMAR 0.5. (B) Preoperative enhanced depth image (EDI) of optical coherence tomography showed folded, distorted retinal thickening with ERM. (C) Preoperative fluorescein angiography showed increasing fluorescence in perimacular area in early phase. (D) Preoperative fluorescein angiography showed hyperfluorescent lesion with blocked fluorescence, vascular distortion with retinal vascular contracting toward the lesion in late phase. (E) Fundus photo at 12 months after membrane peeling, internal limiting membrane peeling, ERM of combined hamartoma of the retina and retinal pigment epithelium was removed. Visual acuity was improved to logMAR 0.1. (F) EDI at 12 months after membrane peeling, internal limiting membrane peeling, central retinal thickness value has decreased 550 µm to 337 µm and subfoveal choroidal thickness value has decreased 203 µm to 191 µm.

Table 1
Baseline characteristics of participants

Values are presented as mean ± SD unless otherwise indicated. ‘Group I’ means ‘Membrane peeling only in patients with combined hamartoma of the retina and retinal pigment epithelium’, ‘Group II’ means ‘Membrane peeling + Internal limiting membrane peeling in patients with combined hamartoma of the retina and retinal pigment epithelium’, ‘Group III’ means ‘Membrane peeling only in patients with idiopathic epiretinal membrane’, and ‘Group IV’ means ‘Membrane peeling + Internal limiting membrane peeling in patients with idiopathic epiretinal membrane’.
PPV = pars plana vitrectomy.
Table 2
Comparison of central retinal thickness using optical coherence tomography

Values are presented as mean ± SD unless otherwise indicated. ‘Group I’ means ‘Membrane peeling only in patients with combined hamartoma of the retina and retinal pigment epithelium’, ‘Group II’ means ‘Membrane peeling + Internal limiting membrane peeling in patients with combined hamartoma of the retina and retinal pigment epithelium’, ‘Group III’ means ‘Membrane peeling only in patients with idiopathic epiretinal membrane’, and ‘Group IV’ means ‘Membrane peeling + Internal limiting membrane peeling in patients with idiopathic epiretinal membrane’.
CRT = central retinal thickness using optical coherence tomography.
*p < 0.05; †Wilcoxon matched pairs signed ranks test; ‡Mann-Whitney test.
Table 3
Comparison of subfoveal choroidal thickness using optical coherence tomography

Values are presented as mean ± SD unless otherwise indicated. ‘Group I’ means ‘Membrane peeling only in patients with combined hamartoma of the retina and retinal pigment epithelium’, ‘Group II’ means ‘Membrane peeling + Internal limiting membrane peeling in patients with combined hamartoma of the retina and retinal pigment epithelium’, ‘Group III’ means ‘Membrane peeling only in patients with idiopathic epiretinal membrane’, and ‘Group IV’ means ‘Membrane peeling + Internal limiting membrane peeling in patients with idiopathic epiretinal membrane’.
SFCT = subfoveal choroidal thickness using optical coherence tomography.
*p < 0.05; †Wilcoxon matched pairs signed ranks test; ‡Mann-Whitney test.
Table 4
Comparison of best corrected visual acuity (logMAR)

Values are presented as mean ± SD unless otherwise indicated. ‘Group I’ means ‘Membrane peeling only in patients with combined hamartoma of the retina and retinal pigment epithelium’, ‘Group II’ means ‘Membrane peeling + Internal limiting membrane peeling in patients with combined hamartoma of the retina and retinal pigment epithelium’, ‘Group III’ means ‘Membrane peeling only in patients with idiopathic epiretinal membrane’, and ‘Group IV’ means ‘Membrane peeling + Internal limiting membrane peeling in patients with idiopathic epiretinal membrane’.
BCVA = best corrected visual acuity.
*p < 0.05; †Wilcoxon matched pairs signed ranks test; ‡Mann-Whitney test.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download