Abstract
Purpose
To report a rare case of a recurrent painless mass of the right lower eyelid, which was histologically diagnosed as a mucinous adenocarcinoma.
Case summary
A 59-year-old male had a painless nodule on the right lower eyelid for 2 years. He had a history of five laser treatments done by a dermatologist prior to the initial presentation. Surgical shave biopsy was performed and a histopathological examination revealed a mucinous adenocarcinoma. We subsequently performed a pentagonal excision of the lower eyelid with assisted frozen biopsy until no tumor cells were seen at the margin. A postoperative whole-body positron emission tomography scan, chest computerized tomography, gastrointestinal endoscopy, and colonoscopy excluded systemic metastases. No recurrence has been observed for 18 months after the surgery.
Conclusions
Primary mucinous adenocarcinoma is a rare disorder of the eyelid. Because it has various morphologies, and the final diagnosis can only be made by histopathological examination. If there is a recurrent mass at the eyelid margin, adenocarcinoma should be considered as the differential diagnosis. A complete surgical excision is recommended to prevent local recurrence.
Figures and Tables
Figure 1
Clinical findings. (A) Preoperative appearance shows erythematous nodule with ulceration on the right lower eyelid. It is firm and non-tender nodule with smooth and shiny surface. The lesion had well-defined margin measuring about 0.7 × 0.6 cm. (B) After 3 weeks, ulceration progressed to the center of the nodule.
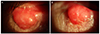
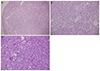
Figure 2
Histopathologic appearance of the surgical specimen. (A) The tumor cells are observed in the subepithelial stroma (Hematoxylin & eosin [H&E] stain, ×100). (B) The tumor shows sheets of atypical cells with abundant cytoplasm and intraluminal mucin with few floating cells (H&E stain, ×200). (C) Photomicrograph shows di-Periodic Acid-Schiff (PAS) positive for intraluminal mucins. Individual tumor cells had a hyperchromatic nucleus (PAS stain, ×200).
Notes
References
1. Chauhan A, Ganguly M, Takkar P, Dutta V. Primary mucinous carcinoma of eyelid: a rare clinical entity. Indian J Ophthalmol. 2009; 57:150–152.

2. Lennox B, Pearse AG, Richards HG. Mucin-secreting tumours of the skin with special reference to the so-called mixed-salivary tumour of the skin and its relation to hidradenoma. J Pathol Bacteriol. 1952; 64:865–880.

3. Mendoza S, Helwig EB. Mucinous (adenocystic) carcinoma of the skin. Arch Dermatol. 1971; 103:68–78.

4. Seo HC, Ahn M, Cho NC, Lee DO. A case of primary mucinous adenocarcinoma of the upper eyelid. J Korean Ophthalmol Soc. 2007; 48:599–603.
5. Hong SM, Kim SD, Yun KJ. A case of primary mucinous adenocarcinoma on skin of the lateral canthus. J Korean Ophthalmol Soc. 2009; 50:1582–1585.

6. Kamalpour L, Brindise RT, Nodzenski M, et al. Primary cutaneous mucinous carcinoma: a systematic review and meta-analysis of outcomes after surgery. JAMA Dermatol. 2014; 150:380–384.
7. Terada T, Sato Y, Furukawa K, Sugiura M. Primary cutaneous mucinous carcinoma initially diagnosed as metastatic adenocarcinoma. Tohoku J Exp Med. 2004; 203:345–348.

8. Carson HJ, Gattuso P, Raslan WF, Reddy V. Mucinous carcinoma of the eyelid. An immunohistochemical study. Am J Dermatopathol. 1995; 17:494–498.

9. Wright JD, Font RL. Mucinous sweat gland adenocarcinoma of eyelid: a clinicopathologic study of 21 cases with histochemical and electron microscopic observations. Cancer. 1979; 44:1757–1768.
10. Liszauer AD, Brownstein S, Codère F. Mucinous eccrine sweat gland adenocarcinoma of the eyelid. Can J Ophthalmol. 1988; 23:17–21.
11. Gardner TW, O'Grady RB. Mucinous adenocarcinoma of the eyelid. A case report. Arch Ophthalmol. 1984; 102:912.
12. Segal A, Segal N, Gal A, Tumuluri K. Mucinous sweat gland adenocarcinoma of the eyelid - current knowledge of a rare tumor. Orbit. 2010; 29:334–340.

13. Zhang Q, Wojno TH, Fitch SD, Grossniklaus HE. Mucinous eccrine adenocarcinoma of the eyelid: report of 6 cases. Can J Ophthalmol. 2010; 45:76–78.

14. Ohnishi T, Takizawa H, Watanabe S. Immunohistochemical analysis of cytokeratin and human milk fat globulin expression in mucinous carcinoma of the skin. J Cutan Pathol. 2002; 29:38–43.
15. Scilletta A, Soma PF, Grasso G, et al. Primary cutaneous mucinous carcinoma of the cheek. Case report. G Chir. 2011; 32:323–325.
16. Miyasaka M, Tanaka R, Hirabayashi K, et al. Primary mucinous carcinoma of the skin: a case of metastasis after 10 years of disease-free interval. Eur J Plast Surg. 2009; 32:189–193.
18. Bellezza G, Sidoni A, Bucciarelli E. Primary mucinous carcinoma of the skin. Am J Dermatopathol. 2000; 22:166–170.

19. Hemalatha AL, Kausalya SK, Amita K, et al. Primary mucinous eccrine adenocarcinoma–A rare malignant cutaneous adnexal neoplasm at an unconventional site. J Clin Diagn Res. 2014; 8:FD14–FD15.
20. Krishnakumar S, Rambhatla S, Subramanian N, et al. Recurrent mucinous carcinoma of the eyelid. Indian J Ophthalmol. 2004; 52:156–157.
21. Lee GA, Cominos D, Sullivan TJ. Clinicopathological report: mucinous carcinoma of the eyelid. Aust N Z J Ophthalmol. 1999; 27:71–73.

22. Grossman JR, Izuno GT. Primary mucinous (adenocystic) carcinoma of the skin. Arch Dermatol. 1974; 110:274–276.

23. Boi S, De Concini M, Detassis C. Mucinous sweat-gland adenocarcinoma of the inner canthus: a case report. Ann Ophthalmol. 1988; 20:189–190.
24. Tak MS, Cho SE, Kang SG, et al. Primary cutaneous mucinous carcinoma of the eyelid. Arch Craniofac Surg. 2016; 17:176–179.

25. Choi JH, Kim SC, Kim J, Chung YK. Primary cutaneous mucinous carcinoma treated with narrow surgical margin. Arch Craniofac Surg. 2016; 17:158–161.

26. Chavez A, Linos K, Samie FH. Primary cutaneous mucinous carcinoma of the eyelid treated with Mohs surgery. JAAD Case Rep. 2015; 1:85–87.

27. Bindra M, Keegan DJ, Guenther T, Lee V. Primary cutaneous mucinous carcinoma of the eyelid in a young male. Orbit. 2005; 24:211–214.

28. Maerki J, Ahmed S, Lee E. Primary mucinous carcinoma of the skin. Eplasty. 2013; 13:ic47.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download