Abstract
Purpose
To analyze the characteristics of medical disputes relating to ophthalmology for prevention in advance.
Methods
Retrospective analyses of ophthalmic cases applied for Korea Medical Dispute Mediation and Arbitration Agency between June 2013 and September 2016.
Results
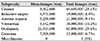
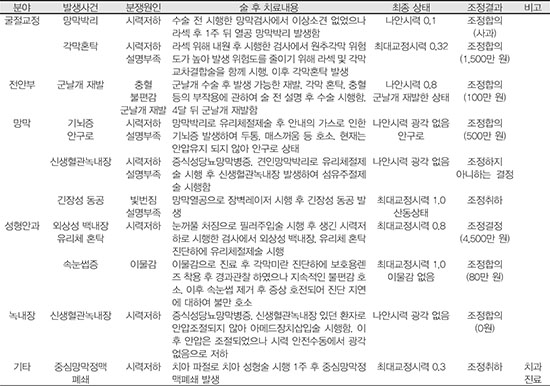
A total of 41 cases were analyzed. The number of cases relating to cataract were 19 (46.3%), refractive surgery 4 (9.8%), anterior segment 4 (9.8%), retina 7 (17.1%), oculoplasty 3 (7.3%), glaucoma 2 (4.9%), and miscellaneous 2 (4.9%). The specialty with the lowest mean payment of mediation per case was cataract (₩3,591,700), which has the largest number of cases, and oculoplasty was the highest mean payment per case (₩21,933,000). There were 16 cases confirmed as negligence by authenticators. Among these 16 cases, 7 (44%) were related to accident during surgery or procedure, 5 cases (31%) were insufficient explanation, and 4 cases (25%) were lack of tests which should have be performed before or after surgery. The results of mediation were agreement in 25 cases (61%), decision made by mediation department in 6 cases (15%), 7 cases were not adequate to mediate (17%), and 3 cases were canceled (7%).
Conclusions
The number of cases associated with cataract was the largest. Among negligence of doctors, cases during surgery were most common, suggesting the need to explain surgical factors such as complications or side effects and the need for complete surgical records. If a medical dispute occurs, the Korea Medical Dispute Mediation and Arbitration Agency can be used to achieve an agreement.
Figures and Tables
Figure 1
Graph showing severity of ophthalmic claims, graded using national patient safety agency severity of outcome scale. It shows relatively high frequency of scales of moderate or more cases. None = no harm; Mild = minimal harm necessitating extra observationor minor treatment; Moderte = significant, but not permanent harm, or moderate increase in treatment; Severe = permanent harm resulting from the incident; Death = death resulting from the incident.
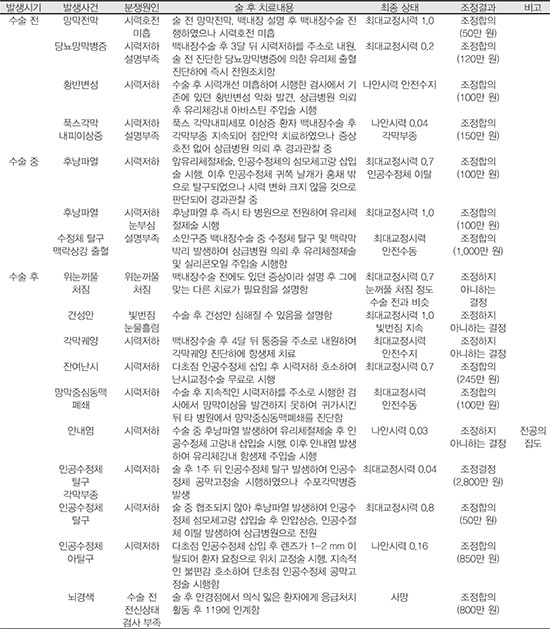
Figure 2
Classification of negligence identified by authenticators among cases of medical dispute relating to ophthalmology. Accident during surgery showed highest frequency among negligence.

Figure 3
Results of mediation associated with ophthalmology. Many cases were resolved by Korea medical dispute and arbitration agency. Agreement of mediation = mutual agreement made between the individuals involved. Mediation department follows the decision; Decision of mediation = the discision made by mediation department, when the agreement of mediation fails, that is thought to be most reasonable; Cases not adequate to mediate = cases that is not thought to be suitable for mediation by the mediation department.

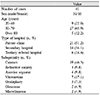
Table 1
National patient safety agency severity of outcome scale for patient safety incidents

*First aid, additional therapy, or additional medication; excludes extra stay in hospital, return to surgery, or readmission; †Return to surgery, unplanned readmission, prolonged episode of care as inpatient or out-patient, or transfer to another area such as intensive care; ‡Permanent reduction of bodily functions: sensory, motor, physiological, or intellectual.
References
1. Hwang JM, Kim KR, Lee KK, et al. Medical disputes in field of ophthalmology. 1st ed. Seoul: Sinjosa;2016. p. 27.
2. Shin EJ. The perspective of the system on mediation in the act of medical malpractice damage's relief and mediation for medical dispute resolution. Korean J Med Law. 2011; 19:133–159.
3. Korea Medical Dispute Mediation and Arbitration Agency. Medical dispute mediation and arbitration statistical yearbook 2015. Accessed March 5, 2017. https://www.k-medi.or.kr/lay1/bbs/S1T27C96/A/25/view.do?article_seq=2614&cpage=&rows=&condition=&keyword=.
4. Mathew RG, Ferguson V, Hingorani M. Clinical negligence in ophthalmology: fifteen years or National Health Service litigation authority data. Ophthalmology. 2013; 120:859–864.
6. Yoo YJ, Lee KK, Hwang JM. Litigations in ophthalmology for 25 years in Korea. J Korean Ophthalmol Soc. 2015; 56:1104–1110.

7. Ali N, Little BC. Causes of cataract surgery malpractice claims in England 1995-2008. Br J Ophthalmol. 2011; 95:490–492.

8. Bhan A, Dave D, Vernon SA, et al. Risk management strategies following analysis of cataract negligence claims. Eye (Lond). 2005; 19:264–268.

9. Gallagher TH, Waterman AD, Ebers AG, et al. Patients' and physicians' attitudes regarding the disclosure of medical errors. JAMA. 2003; 289:1001–1007.

10. General Medical Council. Good Medical Practice. London: GMC;1998. 18. Accessed March 5, 2017. https://www.gmc-uk.org/good_medical_practice_july_1998.pdf_25416527.pdf.
11. Bunting RF Jr, Benton J, Morgan WD. Practical risk management principles for physicians. J Healthc Risk Manag. 1998; 18:29–53.

12. Levinson W, Roter DL, Mullooly JP, et al. Physician-patient communication. The relationship with malpractice claims among primary care physicians and surgeons. JAMA. 1997; 277:553–559.

13. Kim YK. A study on medical malpractice liability insurance, etc. Judical Aff Rev. 2014; 2:53–100.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download