Abstract
Purpose
To report cases of a retinal, preretinal and vitreous hemorrhage due to retinoic acid syndrome and a papilledema caused by increased intracranial pressure in patients with acute promyelocytic leukemia treated with all-trans retinoic acid (ATRA).
Case summary
(Case 1) A 48-year-old female visited our clinic with headache, dyspnea, and visual disturbance during ATRA medications for acute promyelocytic leukemia. Her visual acuity of both eyes was hand motion, and fundus examination revealed extensive retinal, preretinal, and vitreous hemorrhage. The laboratory test showed leukocytosis and computed tomography of brain and chest revealed subarachnoid hemorrhage and pulmonary alveolar hemorrhage. She was diagnosed with retinoic acid syndrome and was treated with vitrectomy in both eyes. (Case 2) A 17-year-old male, who had been treated with ATRA for acute promyelocytic leukemia, had headache and visual disturbance. His best-corrected visual acuity was 1.0 in both eyes, but the fundus examination showed papilledema and retinal hemorrhage in both eyes. Goldmann visual field examination revealed an enlarged blind spot in both eyes. He was diagnosed with papilledema caused by ATRA induced increased intracranial pressure, and was observed.
Figures and Tables
Figure 1
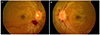
Case 1. (A, B) Fundus photography showed extensive retinal, preretinal, and vitreous hemorrhage in both eyes. (C) The brain computed tomography showed subtle focal high density (red arrow) at left frontal lobe sulcus due to subarachnoid hemorrhage. (D) A contrast-enhanced chest computed tomography revealed patchy ground-glass opacity lesions (green arrow) in the right lower lobe suggesting pulmonary alveolar hemorrhage.

Figure 2
Six months after pars plana vitrectomy in case 1. (A, B) Fundus photography showed relatively stable appearance, and optical coherence tomography revealed foveal atrophy in both eyes.

References
1. Tallman MS, Kwaan HC. Reassessing the hemostatic disorder associated with acute promyelocytic leukemia. Blood. 1992; 79:543–553.
2. Bennett JM, Catovsky D, Daniel MT, et al. French-American-British (FAB) co-operative group. Proposals for the classification of the acute leukaemias. Br J Haematol. 1976; 33:451–458.
3. Larson RA, Kondo K, Vardiman JW, et al. Evidence for a 15;17 translocation in every patient with acute promyelocytic leukemia. Am J Med. 1984; 76:827–841.
4. Koeffler HP. Induction of differentiation of human acute myelogenous leukemia cells: therapeutic implications. Blood. 1983; 62:709–721.
5. Huang ME, Ye YC, Chen SR, et al. Use of all-trans retinoic acid in the treatment of acute promyelocytic leukemia. Blood. 1988; 72:567–572.
6. Fenaux P, Chastang C, Chomienne C, Degos L. European APL Group. Tretinoin with chemotherapy in newly diagnosed acute promyelocytic leukaemia. Lancet. 1994; 343:1033.
7. Frankel SR, Eardley A, Heller G, et al. All-trans retinoic acid for acute promyelocytic leukemia. Results of the New York Study. Ann Intern Med. 1994; 120:278–286.
8. Frankel SR, Eardley A, Lauwers G, et al. The “retinoic acid syndrome” in acute promyelocytic leukemia. Ann Intern Med. 1992; 117:292–296.
9. Roytman M, Frumkin A, Bohn TG. Pseudotumor cerebri caused by isotretinoin. Cutis. 1988; 42:399–400.
10. Mahmoud HH, Hurwitz CA, Roberts WM, et al. Tretinoin toxicity in children with acute promyelocytic leukaemia. Lancet. 1993; 342:1394–1395.
11. Yeh YC, Tang HF, Fang IM. Pseudotumor cerebri caused by all-trans-retinoic acid treatment for acute promyelocytic leukemia. Jpn J Ophthalmol. 2006; 50:295–296.
12. De Botton S, Dombret H, Sanz M, et al. The European APL Group. Incidence, clinical features, and outcome of all trans-retinoic acid syndrome in 413 cases of newly diagnosed acute promyelocytic leukemia. Blood. 1998; 92:2712–2718.
13. Warrell RP Jr, de Thé H, Wang ZY, Degos L. Acute promyelocytic leukemia. N Engl J Med. 1993; 329:177–189.
14. Visani G, Bontempo G, Manfroi S, et al. All-trans-retinoic acid and pseudotumor cerebri in a young adult with acute promyelocytic leukemia: a possible disease association. Haematologica. 1996; 81:152–154.
15. Spector RH, Carlisle J. Pseudotumor cerebri caused by a synthetic vitamin A preparation. Neurology. 1984; 34:1509–1511.
16. Holmes D, Vishnu P, Dorer RK, Aboulafia DM. All-trans retinoic acid-induced pseudotumor cerebri during induction therapy for acute promyelocytic leukemia: a case report and literature review. Case Rep Oncol Med. 2012; 2012:313057.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download