Abstract
Case summary
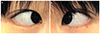
A 27-year-old woman presented to our ophthalmology department with redness and pain in her left eye over 2 days. She received laser-assisted in situ keratomileusis surgery for both eyes 6 years prior and was diagnosed with scleritis in her left eye 3 years prior. She was referred to rheumatologic department to determine if she had auto-immune disease, but the systemic review was negative. She was diagnosed with idiopathic scleritis and was treated with oral Methylprednisolone to provide symptom relief. However, her symptoms exhibited a recurrent pattern. These symptoms regularly affected her during the 2-3 days before menstruation, which had been occurring for more than 10 years, beginning when she was a middle school student. The symptoms affected both eyes and did not improve when treated with topical non-steroid anti-inflammaroty drugs (NSAIDs), topical steroids, or oral NSAIDs. However, her symptoms were relieved when treated with oral steroids. Beginning with her pregnancy and extending through her delivery and breast-feeding periods, follow up had been interrupted, but she noted that recurrence episodes were rare during this time. To this day, her symptoms appear once per month and are controlled through oral steroids.
Conclusions
Literature reviews have revealed no such case reports regarding recurrent scleritis associated with the female menstrual cycle. If cyclic recurrence of scleritis episodes is present in a female patient, a careful history should be taken in order to evaluate any possible associations with the menstrual cycle.
Figures and Tables
References
1. Watson PG, Hayreh SS. Scleritis and episcleritis. Br J Ophthalmol. 1979; 60:163–191.
2. Lin P, Bhullar SS, Tessler HH, Goldstein DA. Immunologic markers as potential predictors of systemic autoimmune disease in patients with idiopathic scleritis. Am J Ophthalmol. 2008; 145:436–471.
3. Foster CS, Sainz de la Maza M. The sclera. 1st ed. New York: Springer Science+Business Media, LLC;1994. 33.
4. Peter W. Disease of the sclera and episclera. In : Duane T, editor. Duane's clinical ophthalmology. revised ed. Philadelphia: Lippincott Williams & Wilkins;1991. v. 4:chap. 23.
5. Fong LP, Sainz de la Maza M, Rice BA, et al. Immunopathology of scleritis. Ophthalmology. 1991; 98:472–479.
6. McCluskey PJ, Watson PG, Lightman S, et al. Posterior scleritis: clinical features, systemic associations, and outcome in a large series of patients. Ophthalmology. 1999; 106:2380–2386.
7. Rajoo SG, Gandhewar J. Recurrent episcleritis in relation to mensturation: a case report. Cornea. 2011; 30:1035–1036.
8. Snell AC. Episcleritis periodica fugax. Trans Am Ophthalmol Soc. 1911; 12(Pt 3):736–745.
9. O'Brien MD. Menstrual red eye. BMJ. 1961; 1:359.
10. Türkçüoğlu I, Türkçüoğlu P, Kurt J, Yildirim H. Presumed nasolacrimal endometriosis. Ophthal Plast Reconstr Surg. 2008; 24:47–48.
11. McGavin DD, Williamson J, Forrester JV, et al. Episcleritis and scleritis. A study of their clinical manifestations and association with rheumatoid arthritis. Br J Ophthalmol. 1976; 60:192–226.
12. Tuft SJ, Watson PG. Progression of scleral disease. Ophthalmology. 1991; 98:467–471.
13. Sainz de la Maza M, Foster CS, Jabbur NS. Scleritis associated with systemic vascullitic diseases. Ophthalmology. 1995; 102:687–692.
14. Hakin KN, Ham J, Lightman SL. Use of orbital floor steroids in the management of patients with uniocular non-necrotising scleritis. Br J Ophthalmol. 1991; 75:337–339.
15. Jabs DA, Mudun A, Dunn JP, Marsh MJ. Episcleritis and scleritis: clinical feartures and treatment results. Am J Ophthalmol. 2000; 130:469–476.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download