Abstract
Purpose
We report a case of one-step operation of persistent pupillary membrane removal, phacoemulsification, and posterior chamber lens implantation that was performed in a patient with persistent pupillary membrane and brunescent cataracts in both eyes.
Case summary
A 64-year-old male with no baseline disease visited our clinic with bilateral decreased visual acuity. His best corrected visual acuity at first visit was 0.1 in the right eye and 0.2 in the left eye. On anterior segment examination, both bilateral persistent pupillary membranes and brunescent cataracts were observed. First, we surgically removed the left pupillary membrane and performed phacoemulsification using posterior chamber lens implantation via one-stage operation. After one week, the same operation was performed for the right eye using the same method. At 6-months postoperative, his best corrected visual acuity was 0.2 in the right eye and 0.8 in the left eye. No complications such as anterior segment inflammation, uveitis, or intraocular pressure elevation were observed during the follow-up period.
Figures and Tables
Figure 1
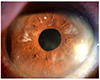
Slit lamp photographs of preoperative persistent pupillary membrane of left eye. (A) Before mydriasis. (B) After mydriasis.

Figure 2
Anterior segment structures as seen under operating microscope showing surgical steps in both eyes. In the left eye, (A) Dispersive ocular viscoelastic device was injected between persistant pupillary membrane and crystalline lens. (B) After appropriate tension to the iris strand was applied by using Phaco Chopper, the operator cut the persistent pupillary mambrane. (C) The remnant iris strands were cut carefully in the same way. (D) Though the persistent pupillary membrane was removed, mydriasis maintained. In the right eye, (E) preopreative persistent pupillary membrane after mydriasis. (F) Mydriasis was also maintained after removing the pupillary membrane.

References
1. Kraus CL, Lueder GT. Clinical characteristics and surgical approach to visually significant persistent pupillary membranes. J AAPOS. 2014; 18:596–599.
2. Lambert SR, Buckley EG, Lenhart PD, et al. Congenital fibrovascular pupillary membranes: clinical and histopathologic findings. Ophthalmology. 2012; 119:634–641.
3. Ko J, Jung JW, Kim EK. Two-stage operation for the treatment of cataract associated with persistent pupillary membrane. J Cataract Refract Surg. 2013; 39:1615.
4. Wang JK, Wu CY, Lai PC. Sequential argon-YAG laser membranectomy and phacoemulsification for treatment of persistent pupillary membrane and associated cataract. J Cataract Refract Surg. 2005; 31:1661–1663.
5. Vega LF, Sabates R. Neodymium: YAG laser treatment of persistent pupillary membrane. Ophthalmic Surg. 1987; 18:452–454.
6. Kumar H, Sakhuja N, Sachdev MS. Hyperplastic pupillary membrane and laser therapy. Ophthalmic Surg. 1994; 25:189–190.
7. Mansour AM, Hamade I, Antonios RS. Sequential argon-YAG laser membranotomy of extensive persistent pupillary membrane with visual loss. BMJ Case Rep. 2015; 2015:pii: bcr2015210140.
8. Kesarwani S, Murthy R, Vemuganti GK. Surgical technique for removing congenital fibrovascular pupillary membrane, with clinicopathological correlation. J AAPOS. 2009; 13:618–620.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download