Abstract
Purpose
To describe the clinical manifestations, treatment results, and antibiotic susceptibility in 6 cases of Stenotrophomonas maltophilia endophthalmitis.
Methods
We retrospectively reviewed 6 eyes of 6 patients who were diagnosed with Stenotrophomonas maltophilia endophthalmitis. Specifically, we considered each patient's age, sex, past history, visual acuity, hypopyon, treatment, and prognosis.
Results
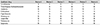
For our study, we considered patients treated during the period of January 2008 to December 2015. Stenotrophomonas maltophilia (6 eyes) was the second most common gram-negative bacteria cause of total bacterial endophthalmitis while Pseudomonas aeruginosa (14 eyes) was the most common gram-negative bacteria cause during the same period. Visual disturbance was the dominant symptom being found in all 6 patients. Other symptoms include ocular pain and hypopyon. The initial visual acuity was light perception (1 patient), hand motion (3 patients), finger count (1 patient), and 0.02 (1 patient). Excluding the 1 patient with light perception, the mean initial visual acuity was logMAR 1.72 (Snellen equivalent; 20/1,049). Overall, 5 patients underwent vitrectomy and intravitreal antibiotics injection, while, the remaining other patient was treated with intravitreal antibiotics injection, followed by vitrectomy. All 6 patients showed sensitivity to Ceftazidime and Levofloxacin and 2 patients showed sensitivity to Trimethoprim/Sulfamethoxazole.
Conclusions
Stenotrophomonas maltophilia endophthalmitis was the second most common gram negative organism to cause endophthalmitis after cataract surgery. All 6 of the tested isolates were found to be sensitive to ceftazidime and levofloxacin. Urgent treatment outcomes were similar to previous reports.
Figures and Tables
Figure 1
Slit lamp photo of case 5. At the time of admission for first vitrectomy, slit lamp photo shows corneal edema and hypopyon.

Figure 2
Fundus photo of case 2. At the time of admission for first vitrectomy, fundus photo shows hazy view due to vitreous opacity.

References
1. Jucker BA, Harms H, Zehnder AJ. Adhesion of the positively charged bacterium Stenotrophomonas (Xanthomonas) maltophilia 70401 to glass and Teflon. J Bacteriol. 1996; 178:5472–5479.
2. Chen S, Stroh EM, Wald K, Jalkh A. Xanthomonas maltophilia endophthalmitis after implantation of sustained-release gancyclovir. Am J Ophthalmol. 1992; 114:772–773.
3. You IC, Lee SH, Park YG, Yoon KC. Clinical aspect and prognosis of stenotrophomonas (xanthomonas) maltophilia keratitis. J Korean Ophthalmol Soc. 2007; 48:889–897.
4. Son SW, Kim HJ, Seo JW. A case of Stenotrophomonas maltophilia keratitis effectively treated with moxifloxacin. Korean J Ophthalmol. 2011; 25:349–351.
5. Seong YS, Koh HJ, Kwon OW. A case of stenotrophomonas maltophilia endophthalmitis after cataract operation. J Korean Ophthalmol Soc. 2001; 42:186–190.
6. Jung JW, Kang HK, Chin HS. Two different cases of stenotrophomonas maltophilia endophthalmitis after cataract surgery. J Korean Ophthalmol Soc. 2012; 53:161–167.
7. Endophthalmitis Vitrectomy Study Group. Results of the Endophthalmitis Vitrectomy Study. A randomized trial of immediate vitrectomy and of intravenous antibiotics for the treatment of postoperative bacterial endophthalmitis. Arch Ophthalmol. 1995; 113:1479–1496.
8. Lange C, Feltgen N, Junker B, et al. Resolving the clinical acuity categories "hand motion" and "counting fingers" using the Freiburg Visual Acuity Test (FrACT). Graefes Arch Clin Exp Ophthalmol. 2009; 247:137–142.
9. Kattan HM, Flynn HW Jr, Pflugfelder SC, et al. Nosocomial endophthalmitis survey. Current incidence of infection after intraocular surgery. Ophthalmology. 1991; 98:227–238.
10. Endophthalmitis Study Group, European Society of Cataract & Refractive Surgeons. Prophylaxis of postoperative endophthalmitis following cataract surgery: results of the ESCRS multicenter study and identification of risk factors. J Cataract Refract Surg. 2007; 33:978–988.
11. Denton M, Kerr KG. Microbiological and clinical aspects of infection associated with Stenotrophomonas maltophilia. Clin Microbiol Rev. 1998; 11:57–80.
12. Kernt M, Kampik A. Endophthalmitis: pathogenesis, clinical presentation, management, and perspectives. Clin Ophthalmol. 2010; 4:121–135.
13. Miño de Kaspar H, Grasbon T, Kampik A. Automated surgical equipment requires routine disinfection of vacuum control manifold to prevent postoperative endophthalmitis. Ophthalmology. 2000; 107:685–690.
14. Brooke JS. Stenotrophomonas maltophilia: an emerging global opportunistic pathogen. Clin Microbiol Rev. 2012; 25:2–41.
15. Gellatly SL, Hancock RE. Pseudomonas aeruginosa: new insights into pathogenesis and host defenses. Pathog Dis. 2013; 67:159–173.
16. Chen KJ, Wang NK, Sun MH, et al. Endophthalmitis caused by Stenotrophomonas maltophilia. Ophthalmic Surg Lasers Imaging. 2010; 41:e555–e561.
17. Chang JS, Flynn HW Jr, Miller D, Smiddy WE. Stenotrophomonas maltophilia endophthalmitis following cataract surgery: clinical and microbiological results. Clin Ophthalmol. 2013; 7:771–777.
18. Eifrig CW, Scott IU, Flynn HW Jr, Miller D. Endophthalmitis caused by Pseudomonas aeruginosa. Ophthalmology. 2003; 110:1714–1717.
19. Sridhar J, Kuriyan AE, Flynn HW Jr, Miller D. Endophthalmitis caused by pseudomonas aeruginosa: Clinical features, antibiotic susceptibilities, and treatment outcomes. Retina. 2015; 35:1101–1106.
20. Horster S, Bader L, Seybold U, et al. Stenotrophomonas maltophilia induced post-cataract-surgery endophthalmitis: outbreak investigation and clinical courses of 26 patients. Infection. 2009; 37:117–122.
21. Penland RL, Wilhelmus KR. Stenotrophomonas maltophilia ocular infections. Arch Ophthalmol. 1996; 114:433–436.
22. Chhablani J, Sudhalkar A, Jindal A, et al. Stenotrophomonas maltophilia endogeneous endophthalmitis: clinical presentation, antiobiotic susceptibility, and outcomes. Clin Ophthalmol. 2014; 8:1523–1526.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download