Abstract
Purpose
Methods
Results
Conclusions
Figures and Tables
Figure 1
Bony nasolacrimal duct (BNLD) measurements with computed tomography (CT). (A) Axial CT image in bone window demonstrates BNLD transverse diameter (yellow line) measurement. (B) It reveals distance between the proximal BNLD (green line). (C) It shows inter-frontozygomatic suture distance (white line).
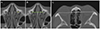
Figure 2
Bony nasolacrimal duct (BNLD) measurements with computed tomography (CT). (A) Sagittal CT image reveals BNLD length (orange line) and proximal, minimal, distal BNLD anteroposterior diameter (yellow lines) measurements, respectively. ‘a’ demonstrates measurement of sagittal orientation angle between long axis (white line) of BNLD and nasal floor (black line). (B) Coronal CT image shows relative lacrimal sac-BNLD orientation angle ‘b’ between long axis of lacrimal sac fossa (green line) and BNLD (white line). ‘c’ reveals angle between long axis of BNLD (white line) and nasal floor (black line). (C) It demonstrates angle (red line) between the bony inferior turbinate and upper part of the medial wall of the maxillary sinus.

Table 1
Patient characteristics

Values are presented as mean ± SD unless otherwise indicated.
PANDO = primary acquired nasolacrimal duct obstruction; SD = standard deviation; M = male; F = female; OD = oculus dexter; OS = oculus sinister.
*No statistical significance using a student t-test; †No statistical significance using a χ2 for independence (p < 0.05).
Table 2
Values of measurements in PANDO side, non-PANDO side, and control groups

Values are presented as mean ± SD unless otherwise indicated.
PANDO = primary acquired nasolacrimal duct obstruction; BNLD = bony nasolacrimal duct; TD = transverse diameter; FZS = frontozygomatic suture; APD = anteroposterior diameter; SD = standard deviation.
*One way analysis of variance (ANOVA) test (p < 0.05). There was no statistically significant difference between PANDO side and non-PANDO side (p > 0.5, Post hoc test).




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download