Abstract
Purpose
We report a case of cryotherapy for fungal corneal ulcers that did not respond to antifungal agents.
Case summary
A 58-year-old man was transferred to our hospital with a left eye corneal ulcer due to pain and visual impairment in his left eye for two weeks, and he was suspected to have a history of fungal infection. At the time of admission, corneal opacity and progressive ulcerative lesions were observed at 5 o'clock in the left eye and visual acuity was 0.025, uncorrected. The corneal ulcer marginal resection, bacterial culture, and potassium hydroxide preparation (KOH) test were performed on lesion sites. Cultures of Candida albicans were reported to grow, topical antibiotics (Fortified tobramycin, Fortified cefazolin, moxifloxacin), and anti-fungal agents (fortified amphotericin B, 0.5%, Natamycin) were administered, but no improvement was observed for 2 weeks. On the 14th day after admission, Cryotherapy was performed. After surgery, eye drops were equally applied, and there was no other discomfort other than pain for 3 days after the operation. He discharged 10 days after surgery, the corneal lesion was healed and the visual acuity was improved to 0.32, uncorrected.
Figures and Tables
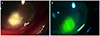 | Figure 1Anterior segment photo of the patient who did not show improvement in medical treatment for 2 weeks. 2 weeks after medical treatment, (A) corneal opacity and progressive infiltrative lesion still observed at 5 o'clock in the left eye. (B) Cornea epithelial defect with ulcerative lesion observed in the cornea at 5 o'clock after stining. |
References
1. Hahn YH, Lee DJ, Kim MS, et al. Epidemiology of Fungal Keratitis in Korea: a multi-center study. J Korean Ophthalmol Soc. 2000; 41:1499–1508.
2. O'Day DM. Selection of appropriate antifungal therapy. Cornea. 1987; 6:238–245.
3. Thomas PA. Fungal infections of the cornea. Eye (Lond). 2003; 17:852–862.
4. Rosa RH Jr, Miller D, Alfonso EC. The changing spectrum of fungal keratitis in south Florida. Ophthalmology. 1994; 101:1005–1013.
5. Lalitha P, Prajna NV, Kabra A, et al. Risk factors for treatment outcome in fungal keratitis. Ophthalmology. 2006; 113:526–530.
6. Xie L, Zhai H, Shi W. Penetrating keratoplasty for corneal perforations in fungal keratitis. Cornea. 2007; 26:158–162.
7. Chen Y, Yang W, Gao M, et al. Experimental study on cryotherapy for fungal corneal ulcer. BMC Ophthalmol. 2015; 15:29.
8. Arora S, Tyragi SC. Fungal flora of conjunctival sac in health and disease. Indian J Ophthalmol. 1976; 24:15–18.
9. Ando N, Takatori K. Fungal flora of the conjunctival sac. Am J Ophthalmol. 1982; 94:67–74.
10. Wilson LA, Ahearn DG, Jones DB, Sexton RR. Fungi from the normal outer eye. Am J Ophthalmol. 1969; 67:52–56.
11. Alfonso EC, Rosa RH, Miller D. Fungal keratitis. In : Krachmer JH, Mannis MJ, Holland EJ, editors. Cornea. 3rd ed. Vol. 1. New York: Mosby Elsevier Inc;2011. chap. 82.
12. Ghannoum MA, Rice LB. Antifungal agents: mode of action, mechanisms of resistance, and correlation of these mechanisms with bacterial resistance. Clin Microbiol Rev. 1999; 12:501–517.
13. Lee KH, Ghae HJ, Yoon KC. Analysis of risk factors for treatment failure in fungal keratitis. J Korean Ophthalmol Soc. 2008; 49:737–742.
14. Mannis MJ. Conjunctival flaps. Int Ophthalmol Clin. 1988; 28:165–168.
15. Sullivan JH. Cryosurgery in ophthalmic practice. Ophthalmic Surg. 1979; 10:37–41.
16. Wilkes TD, Fraunfelder FT. Principles of cryosurgery. Ophthalmic Surg. 1979; 10:21–30.
17. Ebrahimi KB, Green WR, Grebe R, Jun AS. Acanthamoeba sclerokeratitis. Graefes Arch Clin Exp Ophthalmol. 2009; 247:283–286.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download