Abstract
Methods
A retrospective medical record review was conducted on patients that were clinically diagnosed with peripunctal tumor from October 2005 to June 2011 in Dong-A University Hospital.
Results
Twenty nine peripunctal tumors were identified. Five cases (17.2%) were involving upper eyelid and 22 cases (75.9%) were involving lower eyelid. Two cases (6.9%) were involving both upper and lower eyelid, which one of them were involving the conjunctiva as well. One of the patients (3.5%), underwent simple observation without surgery. Simple surgical resection and biopsy were performed in 7 cases (24.1%), and additional silicone tube intubation or Minimonoka insertion were carried-out in 21 cases (72.4%). Histology revealed 15 cases (53.6%) of melanocytic nevus, 5 cases (17.9%) of basal cell carcinoma, 2 cases (7.1%) of seborrheic keratosis, and others including malignant melanoma, squamous papilloma, epidermal cyst, and et cetra.
Conclusions
In conclusion, Peripunctal tumors are mostly found on the lower lids and, they are surgical resection and biopsy should be considered in all cases of peripunctal tumors since they have a potential for spreading to the lacrimal system. It is advised to perform a silicone tube intubation or minimonoka insertion along with the surgical excision to preserve the function of the punctum.
Figures and Tables
Figure 2
Seborrheic keratitis (Table 1, case 25). (A) The photograph of 4 × 4 mm sized, papillary, pigmented mass protruding from the right lower lid, medial to the punctum, 1 mm apart. (B) After 1 week, a postoperative photograph of the patient shows good healing and complete removal of the tumor. (C) Pathologic finding: Histological section shows Keratin-filled invaginations of the epithelium (H&E stain, ×40).
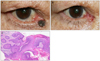
Figure 3
Melanocytic nevus (Table 1, case 12). (A) The photograph of 3 × 2 mm sized, pigmented mass of the left lower lid, lateral to the punctum, 1 mm apart. (B) After 1 month, a postoperative photograph of the patient shows good healing and no recurrence of the tumor. (C) Pathologic finding: Pigmented nevus cells are found in deep and superficial stromal layers (H&E stain, ×100).
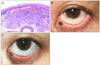
Figure 4
Squamous papilloma (Table 1, case 25). (A) The photograph of 1 × 1 mm sized, papillary mass of the conjunctiva of the left lower lid, near the punctum. (B) After 2 weeks, a postoperative photograph of complete resection and silicone tube well intubated. (C) Pathologic finding: Histological section shows stratified squamous epithelium (H&E stain, ×400).
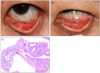
Table 1
The clinical and histopathological data of patients with peripunctal tumors

RUL = right upper lid; RLL = right lower lid; LUL = left upper lid; LLL = left lower lid.
*Even after the surgery, some part of the tumor remained unresected. However, no further resection was carried out; †The size of the tumor was immeasurable because the tumor was spread throughout to the upper lid, lower lid, and conjunctiva.
References
1. Annual report of the Giza Memorial Ophthalmic Laboratory, Annual Report 5. 1931. Cairo, Egypt: Schindler Press;35.
2. Khan JA, Grove AS Jr, Joseph MP, et al. Sebaceous carcinoma, Diuretic use, lacrimal system spread, and surgical margins. Ophthal Plast Reconstr Surg. 1989. 5:227–234.
3. Morel X, Meyer A, Le Rouic JF, et al. [Nevus mimicking a basal cell carcinoma of the eyelid]. J Fr Ophtalmol. 2002. 25:657–660. (Article in French).
4. Pe'er J, Neufeld M, Ilsar M. Peripunctal eyelid oncocytoma. Am J Ophthalmol. 1993. 116:385–387.
5. Scott KR, Jakobiec FA, Font RL. Peripunctal melanocytic nevi. Distinctive clinical findings and differential diagnosis. Ophthalmology. 1989. 96:994–998.
6. Vrabec J. [Naevus puncti lacrimalis]. Sb Lek. 1966. 68:274–278.
7. Imaizumi M, Nakatsuka K. Oncocytoma of the peripunctum. Int Ophthalmol. 2005. 26:111–113.
8. Rumelt S, Pe'er J, Rubin PA. The clinicopathological spectrum of benign peripunctal tumours. Graefes Arch Clin Exp Ophthalmol. 2005. 243:113–119.
9. Welch RB, Duke JR. Lesions of the lids; a statistical note. Am J Ophthalmol. 1958. 45:415–426.
10. Aurora AL, Blodi FC. Reappraisal of basal cell carcinoma of the eyelids. Am J Ophthalmol. 1970. 70:329–336.
11. Tesluk GC. Eyelid lesions: incidence and comparison of benign and malignant lesions. Ann Ophthalmol. 1985. 17:704–707.
12. Folberg R, Jakobiec FA, Bernardino VB, Iwamoto T. Benign conjunctival melanocytic lesions. Clinicopathologic features. Ophthalmology. 1989. 96:436–461.
13. Kersten RC, Ewing-Chow D, Kulwin DR, et al. Accuracy of clinical diagnosis of cutaneous eyelid lesions. Ophthalmology. 1997. 104:479–484.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download