Abstract
Purpose
To describe a case of severe bilateral visual loss in a patient with olfactory groove meningioma.
Case summary
A 64-year-old man presented with a 1-year history of anosmia, progressive loss of vision and visual field deficit. Presenting visual acuity was Counting fingers at 10 cm, and visual field exam showed total visual field defect in both eyes, but there was no remarkable finding to warrant an ophthalmologic examination except mild nucleosclerosis in both eyes and temporal pallor in the left optic nerve head. A brain MRI scan was performed and revealed an olfactory groove meningioma. Surgical resection was performed, and pathologic findings showed meningotheliomatous meningioma. Two months later, the patient was healthy, but no significant improvement of visual acuity or visual field was observed.
Figures and Tables
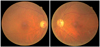
Figure 2
Fundus photographs showing non-specific finding except mild temporal pallor of the left optic disc head.
References
1. McDermott MW, Wilson CB. Youmans JR, editor. Meningiomas. Neurological Surgery. 1996. 4th ed. Philadelphia: Saunders;2782–2825.
2. Rachlin JR, Rosenblum ML. Al-Mefty O, editor. Etiology and biology of meningiomas. Meningiomas. 1991. New York: Raven Press;27–35.
3. Cushing H, Eisenhart L. Meningiomas: Their Classification, Regional Behaviour, Life History, and Surgical End Results. 1938. Springfield, IL: Thomas.
4. Ojemann RG. Al-Mefty O, editor. Olfactory groove meningiomas. Meningiomas. 1991. New York: Raven Press;383–393.
5. Turazzi S, Cristofori L, Gambin R, et al. The pterional approach for the microsurgical removal of olfactory groove meningiomas. Neurosurgery. 1999. 45:821–825.
6. Paterniti S, Fiore P, Levita A, et al. Basal meningiomas. A retrospective study of 139 surgical cases. J Neurosurg Sci. 1999. 43:107–113.
7. Mayfrank L, Gilsbach JM. Interhemispheric approach for microsurgical removal of olfactory groove meningiomas. Br J Neurosurg. 1996. 10:541–545.
8. Tsikoudas A, Martin-Hirsch DP. Olfactory groove meningiomas. Clin Otolaryngol Allied Sci. 1999. 24:507–509.
9. Bakay L. Olfactory meningiomas. The missed diagnosis. JAMA. 1984. 251:53–55.
10. Slavin ML. Acute, severe, symmetric visual loss with cecocentral scotomas due to olfactory groove meningioma. J Clin Neuroophthalmol. 1986. 6:224–227.
11. Welge-Luessen A, Temmel A, Quint C, et al. Olfactory function in patients with olfactory groove meningioma. J Neurol Neurosurg Psychiatry. 2001. 70:218–221.
12. Tuna H, Bozkurt M, Ayten M, et al. Olfactory groove meningiomas. J Clin Neurosci. 2005. 12:664–668.
13. Andrews BT, Wilson CB. Suprasellar meningiomas: the effect of tumor location on postoperative visual outcome. J Neurosurg. 1988. 69:523–528.
14. Zevgaridis D, Medele RJ, Müller A, et al. Meningiomas of the sellar region presenting with visual impairment: impact of various prognostic factors on surgical outcome in 62 patients. Acta Neurochir (Wien). 2001. 143:471–476.
15. Rosenstein J, Symon L. Surgical management of suprasellar meningioma. Part 2: Prognosis for visual function following craniotomy. J Neurosurg. 1984. 61:642–648.
16. Gazzeri R, Galarza M, Gazzeri G. Giant olfactory groove meningioma: ophthalmological and cognitive outcome after bifrontal microsurgical approach. Acta Neurochir (Wien). 2008. 150:1117–1125.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download