Abstract
Purpose
To evaluate prognostic factors for improvement of visual acuity after intravitreal triamcinolone acetonide injection (IVTA) for treatment of macular edema (ME) secondary to branch retinal vein occlusion (BRVO).
Methods
Sixty-eight eyes of 68 consecutive patients treated with IVTA for ME due to BRVO were retrospectively reviewed. Patients were categorized into 2 groups according to the final visual acuity. The 'gainer group' consisted of eyes with a gain of 2 or more Snellen chart lines and the 'non-gainer group' consisted of eyes with less than 2 lines improvement or which had worsened at the last follow-up visit. Comparative clinical characteristics and ophthalmoscopic examinations were analyzed between the 2 groups.
Results
Out of the 68 eyes, 38 (56%) showed improved vision and were categorized as the gainer group; 30 eyes (44%) were categorized as the non-gainer group. The duration of symptoms in the non-gainer group was longer than the gainer group. Additionally, patients with a better baseline vision were expected to show greater improvement. The number of early visual acuity gainers who showed visual improvement at 1 month after IVTA was significantly higher in the gainer group. The number of eyes with angiographically documented macular ischemia was significantly higher in the non-gainer group. Existence of subretinal fluid has been identified as a positive factor for visual improvement.
Figures and Tables
 | Figure 1Parameters evaluated in baseline OCT scans. (A) Height of Subretinal fluid (SRF). (B)Maximum horizontal diameter of intraretinal cystoid spaces (ICS). |
 | Figure 2Changes in logMAR visual acuity after treatment. Within each treatment group, pairwise comparisons revealed significant improvement in visual acuity at each follow-up visit in gainer group (all p < 0.001), whereas a significant change in visual acuity was observed only at post-treatment 2 months in the non-gainer group (p = 0.001). In both groups, the average visual acuity showed improvement at 2 weeks; however, at one month, the tendency toward improved was maintained in the gainer group, and visual acuity showed a slight worsening in the non-gainer group. The asterisk (*) indicates a statistically significant difference within groups (*p < 0.05). |
 | Figure 3Changes in central macular thickness after treatment. The baseline central macular thickness (mean ± SD) was 480.3 ± 181.0 µm in the gainer group and 519.4 ± 138.3 µm in the non-gainer group (p = 0.332). Within each treatment group, pairwise comparisons revealed significant reductions in central macular thicknesses at all time points in both treatment groups (p < 0.05). In both groups, the average central macular thickness showed a gradual decrease afterward at all time points and the mean changes were 247.4 ± 29.5 µm in the gainer group and 165.0 ± 187.2 µm in the non-gainer group at the last follow-up visit. |
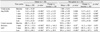
Table 1
Patients' baseline characteristics

Values are mean ± SD or number (%).
SD = standard deviation; HTN = hypertension; V/A = visual acuity; CMT = central macular thickness; IOP = intraocular pressure; IVTA = intravitreal triamcinolone acetonide.
*Student's t-test, †Chi-square test, ‡Fischer's exact test; §from onset of symptoms to the date of first IVTA; ∥from the date after the first IVTA, #Statistically significant result (p < 0.05).
References
1. Greer DV, Constable IJ, Cooper RL. Macular oedema and retinal branch vein occlusion. Aust J Ophthalmol. 1980. 8:207–209.
2. The Branch Vein Occlusion Study Group. Argon laser photocoagulation for macular edema in branch vein occlusion. Am J Ophthalmol. 1984. 98:271–282.
3. Klein R, Klein BE, Moss SE, et al. The Wisconsin epidemiologic study of diabetic retinopathy. IV. Diabetic macular edema. Ophthalmology. 1984. 91:1464–1474.
4. Domalpally A, Blodi BA, Scott IU, et al. The standard care vs corticosteroid for retinal vein occlusion (SCORE) study system for evaluation of optical coherence tomograms: SCORE study report 4. Arch Ophthalmol. 2009. 127:1461–1467.
5. Scott IU, VanVeldhuisen PC, Oden NL, et al. SCORE Study report 1: baseline associations between central retinal thickness and visual acuity in patients with retinal vein occlusion. Ophthalmology. 2009. 116:504–512.
6. Scott IU, Ip MS, VanVeldhuisen PC, et al. A randomized trial comparing the efficacy and safety of intravitreal triamcinolone with standard care to treat vision loss associated with macular edema secondary to branch retinal vein occlusion. Arch Ophthalmol. 2009. 127:1115–1128.
7. Haller JA, Bandello F, Belfort R Jr, et al. Randomized, sham-controlled trial of dexamethasone intravitreal implant in patients with macular edema due to retinal vein occlusion. Ophthalmology. 2010. 117:1134–1146.
8. Campochiaro PA, Heier JS, Feiner L, et al. Ranibizumab for macular edema following branch retinal vein occlusion: six-month primary end point results of a phase III study. Ophthalmology. 2010. 117:1102–1112.
9. Russo V, Barone A, Conte E, et al. Bevacizumab compared with macular laser grid photocoagulation for cystoid macular edema in branch retinal vein occlusion. Retina. 2009. 29:511–515.
10. Kim H, Moon S, Kang J, Yoon H. Intravitreal triamcinolone versus bevacizumab for treatment of macular edema secondary to branch retinal vein occlusion. J Korean Ophthalmol Soc. 2010. 51:1071–1076.
11. Byun YJ, Roh MI, Lee SC, Koh HJ. Intravitreal triamcinolone acetonide versus bevacizumab therapy for macular edema associated with branch retinal vein occlusion. Graefes Arch Clin Exp Ophthalmol. 2010. 248:963–971.
12. Wilson CA, Berkowitz BA, Sato Y, et al. Treatment with intravitreal steroid reduces blood-retinal barrier breakdown due to retinal photocoagulation. Arch Ophthalmol. 1992. 110:1155–1159.
13. Aref AA, Scott IU. Management of macular edema secondary to branch retinal vein occlusion: an evidence-based update. Adv Ther. 2011. 28:28–39.
14. Negi AK, Vernon SA, Lim CS, Owen-Armstrong K. Intravitreal triamcinolone improves vision in eyes with chronic diabetic macular oedema refractory to laser photocoagulation. Eye (Lond). 2005. 19:747–751.
15. Jonas JB, Degenring RF, Kamppeter BA, et al. Duration of the effect of intravitreal triamcinolone acetonide as treatment for diffuse diabetic macular edema. Am J Ophthalmol. 2004. 138:158–160.
16. Bashshur ZF, Ma'luf RN, Allam S, et al. Intravitreal triamcinolone for the management of macular edema due to nonischemic central retinal vein occlusion. Arch Ophthalmol. 2004. 122:1137–1140.
17. Karacorlu M, Ozdemir H, Karacorlu S. Intravitreal triamcinolone acetonide for the treatment of chronic pseudophakic cystoid macular oedema. Acta Ophthalmol Scand. 2003. 81:648–652.
18. Karacorlu M, Mudun B, Ozdemir H, et al. Intravitreal triamcinolone acetonide for the treatment of cystoid macular edema secondary to Behçet disease. Am J Ophthalmol. 2004. 138:289–291.
19. Sutter FK, Gillies MC. Intravitreal triamcinolone for radiation-induced macular edema. Arch Ophthalmol. 2003. 121:1491–1493.
20. Scott IU, Flynn HW Jr, Rosenfeld PJ. Intravitreal triamcinolone acetonide for idiopathic cystoid macular edema. Am J Ophthalmol. 2003. 136:737–739.
21. Michels RG, Gass JD. The natural course of retinal branch vein obstruction. Trans Am Acad Ophthalmol Otolaryngol. 1974. 78:OP166–OP177.
22. Tao Y, Jonas JB. Intravitreal triamcinolone. Ophthalmologica. 2011. 225:1–20.
23. Shulman S, Ferencz JR, Gilady G, et al. Prognostic factors for visual acuity improvement after intravitreal triamcinolone injection. Eye (Lond). 2007. 21:1067–1070.
24. Adamis AP. Is diabetic retinopathy inflammatory disease? Br J Ophthalmol. 2002. 86:363–365.
25. Nauck M, Roth M, Tamm M, et al. Induction of vascular endothelial growth factor by platelet-activating factor and platelet-derived growth factor is downregulated by corticosteroids. Am J Respir Cell Mol Biol. 1997. 16:398–406.
26. Chen SD, Sundaram V, Lochhead J, Patel CK. Intravitreal triamcinolone for the treatment of ischemic macular edema associated with branch retinal vein occlusion. Am J Ophthalmol. 2006. 141:876–883.
27. Cekiç O, Chang S, Tseng JJ, et al. Intravitreal triamcinolone injection for treatment of macular edema secondary to branch retinal vein occlusion. Retina. 2005. 25:851–855.
28. Ozkiris A, Evereklioglu C, Erkilic K, Dogan H. Intravitreal triamcinolone acetonide for treatment of persistent macular oedema in branch retinal vein occlusion. Eye (Lond). 2006. 20:13–17.
29. Jonas JB, Martus P, Degenring RF, et al. Predictive factors for visual acuity after intravitreal triamcinolone treatment for diabetic macular edema. Arch Ophthalmol. 2005. 123:1338–1343.
30. Shilling JS, Jones CA. Retinal branch vein occlusion: a study of argon laser photocoagulation in the treatment of macular oedema. Br J Ophthalmol. 1984. 68:196–198.
31. Choi CU, Seo SW, Yang YS. Different effect of IVTA in the management of macular edema secondary to perfusion and ischemic type BRVO. J Korean Ophthalmol Soc. 2007. 48:49–54.
32. Chung EJ, Hong YT, Lee SC, et al. Prognostic factors for visual outcome after intravitreal bevacizumab for macular edema due to branch retinal vein occlusion. Graefes Arch Clin Exp Ophthalmol. 2008. 246:1241–1247.
33. Catier A, Tadayoni R, Paques M, et al. Characterization of macular edema from various etiologies by optical coherence tomography. Am J Ophthalmol. 2005. 140:200–206.
34. Marmor MF. Mechanisms of fluid accumulation in retinal edema. Doc Ophthalmol. 1999. 97:239–249.
35. Yamaguchi Y, Otani T, Kishi S. Serous macular detachment in branch retinal vein occlusion. Retina. 2006. 26:1029–1033.
36. Brasil OF, Smith SD, Galor A, et al. Predictive factors for short-term visual outcome after intravitreal triamcinolone acetonide injection for diabetic macular oedema: an optical coherence tomography study. Br J Ophthalmol. 2007. 91:761–765.
37. Shah SP, Patel M, Thomas D, et al. Factors predicting outcome of vitrectomy for diabetic macular oedema: results of a prospective study. Br J Ophthalmol. 2006. 90:33–36.
38. Yamaike N, Tsujikawa A, Ota M, et al. Three-dimensional imaging of cystoid macular edema in retinal vein occlusion. Ophthalmology. 2008. 115:355–362.
39. Hoeh AE, Ruppenstein M, Ach T, Dithmar S. OCT patterns of macular edema and response to bevacizumab therapy in retinal vein occlusion. Graefes Arch Clin Exp Ophthalmol. 2010. 248:1567–1572.
40. Kondo M, Kondo N, Ito Y, et al. Intravitreal injection of bevacizumab for macular edema secondary to branch retinal vein occlusion: results after 12 months and multiple regression analysis. Retina. 2009. 29:1242–1248.
41. Jaissle GB, Szurman P, Feltgen N, et al. Predictive factors for functional improvement after intravitreal bevacizumab therapy for macular edema due to branch retinal vein occlusion. Graefes Arch Clin Exp Ophthalmol. 2011. 249:183–192.
42. Scott IU, VanVeldhuisen PC, Oden NL, et al. Baseline predictors of visual acuity and retinal thickness outcomes in patients with retinal vein occlusion: Standard Care Versus COrticosteroid for REtinal Vein Occlusion Study report 10. Ophthalmology. 2011. 118:345–352.
43. Oh JY, Seo JH, Ahn JK, et al. Early versus late intravitreal triamcinolone acetonide for macular edema associated with branch retinal vein occlusion. Korean J Ophthalmol. 2007. 21:18–20.
44. Ota M, Tsujikawa A, Murakami T, et al. Foveal photoreceptor layer in eyes with persistent cystoid macular edema associated with branch retinal vein occlusion. Am J Ophthalmol. 2008. 145:273–280.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download