Abstract
Purpose
Oculomotor disturbance is the common manifestation of intracavernous carotid aneurysm cases. Intracavernous carotid aneurysms causing compressive optic neuropathy with no oculomotor disturbance are relatively rare due to their anatomical characteristics. We experienced a case of intracavernous carotid aneurysm which resulted in a shifted supraclinoid segment of the internal carotid artery, presenting with visual loss and visual field defect with no oculomotor disturbance.
Case summary
A 40-year-old woman presented with loss of vision in the right eye. A relative afferent pupillary defect was observed in this eye. Visual field test showed quadranopsia in the right eye. Magnetic resonance imaging revealed that the intracavernous carotid aneurysm had shifted the supraclinoid segment of the internal carotid artery to the superomedial position. The right optic nerve was directly molded by the shifted supraclinoid segment of the internal carotid artery at the point of the bifurcation between the anterior cerebral artery and the middle cerebral artery. A Guglielmi detachable coil (GDC) embolization was performed successfully with no operational complications. Six months after coiling, best corrected visual acuity of the right eye was 1.0, and the visual field defect had recovered in all except the superior temporal field.
Conclusions
Oculomotor disturbance is frequently associated with intracavernous carotid aneurysms. Nevertheless, optic neuropathy without oculomotor disturbance may be the only sign in patients with an intracavernous carotid aneurysm that causes shifting of the supraclinoid segment of the internal carotid artery.
Figures and Tables
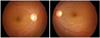 | Figure 1Fundus photographs of the case. The neural rim of the temporal area in the right optic disc appears pale. |
 | Figure 2Initial average and quadrant retinal nerve fiber layer (RNFL) thickness as measured by spectral domain optical coherence tomography. RNFL is thinner in the affected eye compared with the unaffected eye. No significant change is observed after 6 months of GDC coiling treatment. |
 | Figure 3T2-weighted axial (left) and coronal (right) magnetic resonance image. Internal carotid artery aneurysm from its intracavernous segment (A) shifted the supraclinoid segment of the internal carotid artery (B) and basal cistern (C). The right optic nerve (D) is molded by the shifted supraclinoid segment of the internal carotid artery directly on the point of the bifurcation between the middle cerebral artery (E) and the anterior cerebral artery (F). |
 | Figure 4Initial Humphrey visual field test (central 30-2 threshold) shows three quadranopsia in the right eye (A). Subsequent perimetries 6 months after GDC coiling demonstrated improvement of visual field (B). Nevethless the visual field of the right eye at 6 months after coiling still has remnant quadranopsia. |
References
1. Kupersmith MJ, Berenstein A, Choi IS, et al. Percutaneous transvascular treatment of giant carotid aneurysms: neuro-ophthalmologic findings. Neurology. 1984. 34:328–335.
2. Mendez Roberts A, Grimes AL. Enlargement of internal carotid artery aneurysm presenting with severe visual sequela: a case report and anatomy review. Optometry. 2009. 80:76–82.
3. van Rooij WJ, Sluzewski M. Unruptured large and giant carotid artery aneurysms presenting with cranial nerve palsy: comparison of clinical recovery after selective aneurysm coiling and therapeutic carotid artery occlusion. AJNR Am J Neuroradiol. 2008. 29:997–1002.
4. Date I, Asari S, Ohmoto T. Cerebral aneurysms causing visual symptoms: their features and surgical outcome. Clin Neurol Neurosurg. 1998. 100:259–267.
5. Cestari DM, Rizzo JF 3rd. The neuroophthalmic manifestations and treatment options of unruptured intracranial aneurysms. Int Ophthalmol Clin. 2004. 44:169–187.
6. Hahn CD, Nicolle DA, Lownie SP, Drake CG. Giant cavernous carotid aneurysms: clinical presentation in fifty-seven cases. J Neuroophthalmol. 2000. 20:253–258.
7. Vargas ME, Kupersmith MJ, Setton A, et al. Endovascular treatment of giant aneurysms which cause visual loss. Ophthalmology. 1994. 101:1091–1098.
8. Norwood EG, Kline LB, Changdra-Sekar G, Harsh GR 3rd. Aneurysmal compression of the anterior visual pathways. Neurology. 1986. 36:1035–1041.
9. Takahashi T, Kanatani I, Isayama Y, et al. Visual disturbance due to internal carotid aneurysm. Ann Ophthalmol. 1983. 15:1014–1015. 1017–1024.
10. Misra M, Mohanty AB, Rath S. Giant aneurysm of internal carotid artery presenting features of retrobulbar neuritis. Indian J Ophthalmol. 1991. 39:28–29.
11. Guglielmi G, Viñuela F, Dion J, Duckwiler G. Electrothrombosis of saccular aneurysms via endovascular approach. Part 2: Preliminary clinical experience. J Neurosurg. 1991. 75:8–14.
12. Johnston SC, Zhao S, Dudley RA, et al. Treatment of unruptured cerebral aneurysms in California. Stroke. 2001. 32:597–605.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download