Abstract
Purpose
To evaluate the clinical outcomes of visual acuity and foveal thickness after vitrectomy for an idiopathic epiretinal membrane (ERM).
Methods
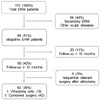
We retrospectively reviewed the records of 62 patients (62 eyes) with ERM who had been treated with vitrectomy between 2004 and 2009. Visual acuity and central macular thickness from optical coherence tomography imaging were obtained preoperatively and at every postoperative follow-up visit.
Results
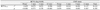
Mean preoperative visual acuity and central macular thickness were 0.495 ± 0.292 log MAR and 414.645 ± 95.528 µm, respectively. Mean visual acuity and central macular thickness 1 month after surgery were 0.389 ± 0.373 log MAR and 341.484 ± 73.676 µm, respectively. Visual acuity improved within 9 months and central macular thickness significantly decreased 12 months after surgery. Most of the changes in visual acuity and central macular thickness took place during the first 3 months. The only parameter which was significantly correlated with final visual acuity was preoperative visual acuity (0.635) (p < 0.001).
Figures and Tables
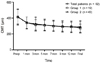
 | Figure 2Changes of best-corrected visual acuity (BCVA) after epiretinal membrane surgery. Group I includes patients who went vitrectomy only and group II consists of patients who went combined surgery (vitrectomy and cataract surgery). Two group did not show significant differences of final visual acuity. log MAR = logarithm of the minimal angle of resolution; Preop = before surgery. |
 | Figure 3Changes of central macular thickness (CMT) after epiretinal membrane surgery. Group I includes patients who went vitrectomy only and group II consists of patients who went combined surgery (vitrectomy and cataract surgery). Two group did not show significant differences of CMT. CMT = central macular thickness; Preop = before surgery. |
References
1. Sidd RJ, Fine SL, Owens SL, Patz A. Idiopathic preretinal gliosis. Am J Ophthalmol. 1982. 94:44–48.
2. Pearlstone AD. The incidence of idiopathic preretinal macular gliosis. Ann Ophthalmol. 1985. 17:378–380.
3. Mitchell P, Smith W, Chey T, et al. Prevalence and associations of epiretinal membranes. The Blue Mountains Eye Study, Australia. Ophthalmology. 1997. 104:1033–1040.
4. Klein R, Klein BE, Wang Q, Moss SE. The epidemiology of epiretinal membranes. Trans Am Ophthalmol Soc. 1994. 92:403–425.
5. Noble KG, Carr RE. Idiopathic preretinal gliosis. Ophthalmology. 1982. 89:521–523.
6. Wise GN. Preretinal macular fibrosis. (An analysis of 90 cases). Trans Ophthalmol Soc U K. 1972. 92:131–140.
7. McDonald HR, Verre WP, Aaberg TM. Surgical management of idiopathic epiretinal membranes. Ophthalmology. 1986. 93:978–983.
8. Machemer R. [The surgical removal of epiretinal macular membranes (macular puckers) (author's transl)]. Klin Monbl Augenheilkd. 1978. 173:36–42.
9. de Bustros S, Thompson JT, Michels RG, et al. Nuclear sclerosis after vitrectomy for idiopathic epiretinal membranes. Am J Ophthalmol. 1988. 105:160–164.
10. Margherio RR, Cox MS Jr, Trese MT, et al. Removal of epimacular membranes. Ophthalmology. 1985. 92:1075–1083.
11. Rice TA, De Bustros S, Michels RG, et al. Prognostic factors in vitrectomy for epiretinal membranes of the macula. Ophthalmology. 1986. 93:602–610.
12. von Gunten S, Pournaras CJ, de Gottrau P, Brazitikos P. [Prognostic factors in surgical treatment of epiretinal membranes]. Klin Monbl Augenheilkd. 1994. 204:309–312.
13. Pesin SR, Olk RJ, Grand MG, et al. Vitrectomy for premacular fibroplasia. Prognostic factors, long-term follow-up, and time course of visual improvement. Ophthalmology. 1991. 98:1109–1114.
14. Trese MT, Chandler DB, Machemer R. Macular pucker. I. Prognostic criteria. Graefes Arch Clin Exp Ophthalmol. 1983. 221:12–15.
15. Poliner LS, Olk RJ, Grand MG, et al. Surgical management of premacular fibroplasia. Arch Ophthalmol. 1988. 106:761–764.
16. de Bustros S, Rice TA, Michels RG, et al. Vitrectomy for macular pucker. Use after treatment of retinal tears or retinal detachment. Arch Ophthalmol. 1988. 106:758–760.
17. Mitamura Y, Hirano K, Baba T, Yamamoto S. Correlation of visual recovery with presence of photoreceptor inner/outer segment junction in optical coherence images after epiretinal membrane surgery. Br J Ophthalmol. 2009. 93:171–175.
18. Suh MH, Seo JM, Park KH, Yu HG. Associations between macular findings by optical coherence tomography and visual outcomes after epiretinal membrane removal. Am J Ophthalmol. 2009. 147:473–480.
19. Kwon SI, Ko SJ, Park IW. The clinical course of the idiopathic epiretinal membrane after surgery. Korean J Ophthalmol. 2009. 23:249–252.
20. Kim J, Rhee KM, Woo SJ, et al. Long-term temporal changes of macular thickness and visual outcome after vitrectomy for idiopathic epiretinal membrane. Am J Ophthalmol. 2010. 150:701–709.
21. Massin P, Allouch C, Haouchine B, et al. Optical coherence tomography of idiopathic macular epiretinal membranes before and after surgery. Am J Ophthalmol. 2000. 130:732–739.
22. Kim CH, Kim JI, Cho HY, Kang SW. Correlation between preoperative OCT pattern and visual improvement in macular epiretinal membrane. J Korean Ophthalmol Soc. 2007. 48:75–82.
23. Michels RG. Vitrectomy for macular pucker. Ophthalmology. 1984. 91:1384–1388.
24. Iwanoff A. Beiträge zur normalen und pathologischen Anatomie des Auges. Graefe's Arch Clin Exp Ophthalmol. 1865. 11:135–170.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download