Abstract
Purpose
To investigate complication rates and results of cataract surgery in a monocular patient compared to normal binocular cataract patients.
Methods
We retrospectively analyzed 84 eyes of 84 patients that had undergone phacoemulsification, intraocular lens implantation and were followed up for 6 months or more. The fellow eye condition was classified into two different groups: Group A (experimental group) and Group B (control group). The best corrected visual acuity (BCVA) before and after surgery, operation time, nucleus sclerosis, and complication rate between the two groups were compared.
Results
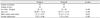
Both groups showed a significant level of visual improvement after 6 months (p < 0.01, 0.01). There was no significant difference in sex, age, preoperative lens opacity, pre- and postoperative visual acuity, spherical equivalent, astigmatism, and rate of complications (posterior capsule rupture [n = 1], uveitis [n = 1] vs. posterior capsule rupture [n = 3], intraocular lens capture [n = 1].
Figures and Tables
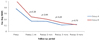
Figure 1
Change of visual acuity after operation. Vac = visual acuity, Preop = preoperative, Postop = postoperative, log MAR = logarithm of the minimal angle of resolution.
References
1. Brian G, Taylor H. Cataract blindness--challenges for the 21st century. Bull World Health Organ. 2001. 79:249–256.
2. Grabow HB. Topical anesthesia for cataract surgery. Eur J Implant Refract Surg. 1993. 5:20–24.
3. Gimbel HV, Neuhann T. Development, advantages, and methods of the continuous circular capsulorhexis technique. J Cataract Refract Surg. 1990. 16:31–37.
4. Dogru M, Honda R, Omoto M, et al. Early visual results with the rollable ThinOptX intraocular lens. J Cataract Refract Surg. 2004. 30:558–565.
5. Pandey SK, Werner L, Agarwal A, et al. Phakonit. cataract removal through a sub-1.0 mm incision and implantation of the ThinOptX rollable intraocular lens. J Cataract Refract Surg. 2002. 28:1710–1713.
6. Alió J, Rodríguez-Prats JL, Galal A, Ramzy M. Outcomes of microincision cataract surgery versus coaxial phacoemulsification. Ophthalmology. 2005. 112:1997–2003.
7. Pingree MF, Crandall AS, Olson RJ. Cataract surgery complications in 1 year at an academic institution. J Cataract Refract Surg. 1999. 25:705–708.
8. Kim KH, Oh TS, Jang SD. Clinical aspects of 273 patients with visual disability. J Korean Ophthalmol Soc. 2002. 43:136–142.
9. Ciulla TA, Starr MB, Masket S. Bacterial endophthalmitis prophylaxis for cataract surgery: an evidence-based update. Ophthalmology. 2002. 109:13–24.
10. Ou JI, Ta CN. Endophthalmitis prophylaxis. Ophthalmol Clin North Am. 2006. 19:449–456.
11. Wong TY, Chee SP. The epidemiology of acute endophthalmitis after cataract surgery in an Asian population. Ophthalmology. 2004. 111:699–705.
12. Lalitha P, Rajagopalan J, Prakash K, et al. Postcataract endophthalmitis in South India incidence and outcome. Ophthalmology. 2005. 112:1884–1889.
13. Choi GJ, Yoon GJ, Na KS. Clinical Observation on Postoperative Endophthalmitis Following Cataract Surgery. J Korean Ophthalmol Soc. 1996. 37:961–966.
14. Lee SB, Han JW, Chung SK, Baek NH. Factors associated with visual outcomes of postoperative endophthalmitis following cataract surgery. J Korean Ophthalmol Soc. 2005. 46:1618–1623.
15. Mamalis N, Edelhauser HF, Dawson DG, et al. Toxic anterior segment syndrome. J Cataract Refract Surg. 2006. 32:324–333.
16. Wilson FM, Wilson FM II. Duane TD, editor. Postoperative uveitis. Clinical Ophthalmology. 1988. 1988. v. 4:Revised ed. Philadelphia: Harper and Row;2–3.
17. Locatcher-Khorazo D, Gutierrez B. Ocular flora of 1,024 children(1~18 years old), 1,786 young adults(20~35 years old) and 7,461 patient : awaiting ocular surgery, with no known infection(Unpublished data from 1952 to 1968), Microbiology of the eye. 1972. Baltimore: CV Mosby;14–16.
18. Choi S, Shin D. Comparison of normal bacterial flora in the conjuntival sac of normal and anophthalmic eyes. J Korean Ophthalmol Soc. 1991. 32:939–943.
19. Sun DY, Lee JH. The lncidence of Retinal Detachment after Cataract Surgery according to Surgical Methods. J Korean Ophthalmol Soc. 1995. 36:2157–2161.
20. Lois N, Wong D. Pseudophakic retinal detachment. Surv Ophthalmol. 2003. 48:467–487.
21. Boberg-Ans G, Villumsen J, Henning V. Retinal detachment after phacoemulsification cataract extraction. J Cataract Refract Surg. 2003. 29:1333–1338.
22. Wilkinson CP, Anderson LS, Little JH. Retinal detachment following phacoemulsification. Ophthalmology. 1978. 85:151–156.
23. Smith PW, Stark WJ, Maumenee AE. Retinal detachment after extracapsular cataract extraction with posterior chamber intraocular lens. Ophthalmology. 1987. 94:495–504.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download