Abstract
Purpose
To report the clinical results after the implantation of intrastromal corneal ring segments (Intacs®) by manual tunnel creation for the correction of keratoconus.
Methods
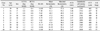
This retrospective case series was comprised of 10 eyes of 8 consecutive keratoconic patients. Visual acuity, refractive outcome, keratometric values, anterior chamber depth, central corneal thickness, and endothelial cell density were evaluated before and at 1 month, 3 months, and 6 months postoperatively. In addition, the implanted ring segment depth was measured by anterior segment optical coherence tomography at postoperative 6 months. Any postoperative complications were also recorded.
Results
Visual acuity was improved in 9 out of 10 eyes. Spherical equivalent and keratometric values were decreased in all eyes. There was no significant difference in central corneal thickness, but endothelial cell density and anterior chamber depth were slightly decreased. The depth of ring segments was almost constant at superior, middle, and inferior. There was a single case of descented implanted ring segments and 6 cases of stromal infiltration around ring segments, but visual acuity was unaffected. In addition, 1 case showed implanted ring exposure, thus the superior ring segment was removed at postoperative 4 months.
Figures and Tables
 | Figure 1Changes of the best corrected visual acuity (BCVA) after intacs implantation. In 9 out of 10 eyes (90%), the BCVA was improved at postoperative 6 months. A gain of 4 or more lines was seen in 6 eyes (60%). |
 | Figure 2Preoperative (left) and postoperative (right) mean keratometric maps of corneal topography 6 months after intacs implantation in case 1, 4, 5. The changes of maximal K are from 57.0 D to 50.0 D in case 1, 49.2 D to 44.6 D in case 4, 49.5 D to 46.4 D in case 5. There is the significant reduction in the K values. |
 | Figure 3Spectral-domain optical coherence tomography cross-section showing the intrastromal corneal ring segment depth at superior (top), middle (middle) and inferior (bottom) portion in case 2. The depth is almost constant. |
 | Figure 4Inferior descent of the implanted ring segments (arrow) occurred at postoperative 2 months in Case 1 but the visual acuity was not affected (A). The lamellar channel deposit in the inner surface of the ring segment (arrow) was observed in 6 cases, however did not influence visual outcomes in all of the cases (B). |
 | Figure 5In case 6, corneal melting was observed at postoperative 4 weeks at the site of knot removal followed by superior implanted ring segment exposure at postoperative 6 weeks (A). We removed the exposed superior ring segment at postoperative 4 months (B). Corneal epithelial defect healed 1 month after removal (C). |
References
1. Krachmer JH, Feder RS, Belin MW. Keratoconus and related noninflammatory corneal thinning disorders. Surv Ophthalmol. 1984. 28:293–322.
2. Rabinowitz YS. Keratoconus. Surv Ophthalmol. 1998. 42:297–319.
3. Kim MK, Lee JH. Long-term outcome of graft rejection after penetrating keratoplasty. J Korean Ophthalmol Soc. 1997. 38:1553–1560.
4. Kim KH, Ahn K, Chung ES, Chung TY. Comparison of deep anterior lamellar keratoplasty and penetrating keratoplasty for keratoconus. J Korean Ophthalmol Soc. 2008. 49:222–229.
5. Wollensak G, Spoerl E, Seiler T. Riboflavin/ultraviolet-a-induced collagen crosslinking for the treatment of keratoconus. Am J Ophthalmol. 2003. 135:620–627.
6. Lee P, Jin KH. Clinical results of riboflavin and ultraviolet-a-induced corneal cross-linking for progressive keratoconus in Korean patients. J Korean Ophthalmol Soc. 2011. 52:23–28.
7. Colin J, Cochener B, Savary G, Malet F. Correcting keratoconus with intracorneal rings. J Cataract Refract Surg. 2000. 26:1117–1122.
8. Siganos CS, Kymionis GD, Kartakis N, et al. Management of keratoconus with Intacs. Am J Ophthalmol. 2003. 135:64–70.
9. Colin J, Malet FJ. Intacs for the correction of keratoconus: two-year follow-up. J Cataract Refract Surg. 2007. 33:69–74.
10. Choi SW, Choae WS, Her J. Intrastromal corneal ring segments (Keraring®) implantation for the correction of keratoconus. J Korean Ophthalmol Soc. 2011. 52:277–284.
11. Ha CI, Choi SK, Lee DH, Kim JH. The clinical results of intrastromal corneal ring segment implantation using a femtosecond laser in keratectasia. J Korean Ophthalmol Soc. 2010. 51:1–7.
12. Kim HS, Lee TH, Lee KH. Intracorneal ring segment implantation for the management of keratoconus: short-term safety and efficacy. J Korean Ophthalmol Soc. 2009. 50:1505–1509.
13. Ertan A, Kamburoğlu G. Intacs implantation using a femtosecond laser for management of keratoconus: Comparison of 306 cases in different stages. J Cataract Refract Surg. 2008. 34:1521–1526.
14. Piñero DP, Alio JL, El Kady B, et al. Refractive and aberrometric outcomes of intracorneal ring segments for keratoconus: mechanical versus femtosecond-assisted procedures. Ophthalmology. 2009. 116:1675–1687.
15. Maguire LJ, Lowry JC. Identifying progression of subclinical keratoconus by serial topography analysis. Am J Ophthalmol. 1991. 112:41–45.
16. Alió JL, Shabayek MH, Belda JI, et al. Analysis of results related to good and bad outcomes of Intacs implantation for keratoconus correction. J Cataract Refract Surg. 2006. 32:756–761.
17. Ruckhofer J, Twa MD, Schanzlin DJ. Clinical characteristics of lamellar channel deposits after implantation of intacs. J Cataract Refract Surg. 2000. 26:1473–1479.
18. Rodrigues MM, McCarey BE, Waring GO 3rd, et al. Lipid deposits posterior to impermeable intracorneal lenses in rhesus monkeys: clinical, histochemical, and ultrastructural studies. Refract Corneal Surg. 1990. 6:32–37.
19. Coskunseven E, Jankov MR 2nd, Hafezi F, et al. Effect of treatment sequence in combined intrastromal corneal rings and corneal collagen crosslinking for keratoconus. J Cataract Refract Surg. 2009. 35:2084–2091.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download