Abstract
Purpose
To evaluate the efficacy, safety, and satisfaction of patients who underwent conductive keratoplasty (CK).
Methods
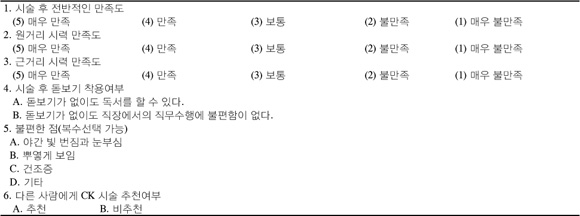
CK was performed in 20 patients between April and December 2009. Surgeries were performed on the dominant eye with emmetropia as the postoperative goal and on the non-dominant eye with mild myopia as the postoperative goal. Patients' satisfaction, refractive change, and visual acuity were evaluated for at least 3 months after the surgery.
Results
Preoperatively, the mean manifest refraction spherical equivalent (MRSE) of the non-dominant and dominant patient eyes was 0.56 ± 0.48 D and 0.88 ± 0.25 D, respectively. Postoperatively, the mean MRSE of the non-dominant and dominant patient eyes was -1.65 ± 0.56 D and -0.06 ± 0.36D at 1 month, -1.33 ± 0.40 D and 0.17 ± 0.37 D at 3 months, and -1.10 ± 0.44 D and 0.31 ± 0.33 D at 6 months, respectively, indicating significant effect regression. Eleven out of 20 patients (55%) were disappointed with the results of CK.
Figures and Tables
Figure 1
Perioperative changes in mean and standard deviation of spherical equivalent (SE) over 6 months of follow-up after conductive keratoplasty.
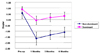
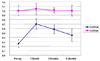
Figure 2
Preoperative (A) and 1-(B) and 6-months (C) postoperative corneal topographic change in a patient who underwent CK. Postoperative topography shows a generally prolate optical contour with central steepening and relative flattening in the mid-periphery.

References
1. Kim MG, Kim TJ, Park YG, et al. Lee YS, et al. Presbyopic Contact Lens Fitting. Contact lens: Principles and practice. 2007. 1st ed. Seoul: Naewae haksool;v.1. chap.14.
2. Mantry S, Shah S. Surgical management of presbyopia. Cont Lens Anterior Eye. 2004. 27:171–175.
3. Lee HY, Her J. Clinical evaluation of monovision after cataract surgery. J Korean Ophthalmol Soc. 2008. 49:1437–1442.
4. Stahl JE. Conductive keratoplasty for presbyopia: 1-year results. J Refract Surg. 2006. 22:137–144.
5. Stahl JE. Conductive keratoplasty for presbyopia: 3-year results. J Refract Surg. 2007. 23:905–910.
6. Habibollahi A, Hashemi H, Mehravaran S, Khabazkhoob M. Visual Outcomes of conductive keratoplasty to treat hyperopia and astigmatism after laser in situ keratomileusis and photorefractive keratectomy. Middle East Afr J Ophthalmol. 2011. 18:238–242.
7. Chang JS, Lau SY. Conductive keratoplasty to treat hyperopic overcorrection after LASIK for myopia. J Refract Surg. 2011. 27:49–55. doi: 10.3928/1081597X-20100212-10. Epub 2010 Feb 15.
8. Jin YH, Moon NJ, Seong PJ. Refraction and Prescription. 2009. 3rd ed. Seoul: Naewae haksool;125–140.
9. Duane A. Subnormal accommodation. Trans Am Ophthalmol Soc. 1925. 23:159–183.
10. Duke-Elder S. System of Ophthalmology. 1970. Vol. 5:1st ed. St. Louis: CV Mosby;484.
11. Harris MG, Classé JG. Clinicolegal considerations of monovision. J Am Optom Assoc. 1988. 59:491–495.
12. Jain S, Arora I, Azar DT. Success of monovision in presbyopes: review of the literature and potential applications to refractive surgery. Surv Ophthalmol. 1996. 40:491–499.
13. Ahn K, Huh DW, Kim WJ, Chung ES. Clinical evaluationnof monovision induced by laser thermal keratoplasty (LTK). J Korean Ophthalmol Soc. 2003. 44:1036–1043.
14. du Toit R, Ferreira JT, Nel ZJ. Visual and nonvisual variables implicated in monovision wear. Optom Vis Sci. 1998. 75:119–125.
15. Greenbaum S. Monovision pseudophakia. J Cataract Refract Surg. 2002. 28:1439–1443.
16. Lans LJ. Experimentelle untersuchungen über entstehung von astigmatismus durch nicht-perforirende corneawunden. Graefes Arch Clin Exp Ophthalmol. 1898. 45:117–152.
17. Neumann AC, Fyodorov S, Sanders DR. Radial thermokeratoplasty for the correction of hyperopia. Refract Corneal Surg. 1990. 6:404–412.
18. Feldman ST, Ellis W, Frucht-Pery J, et al. Regression of effect following radial thermokeratoplasty in humans. Refract Corneal Surg. 1989. 5:288–291.
19. Peyman GA, Larson B, Raichand M, Andrews AH. Modification of rabbit corneal curvature with use of carbon dioxide laser burns. Ophthalmic Surg. 1980. 11:325–329.
20. Naoumidi TL, Pallikaris IG, Naoumidi II, Astyrakakis NI. Conductive Keratoplasty: histological study of human corneas. Am J Ophthalmol. 2005. 140:984–992.
21. Haw WW, Manche EE. Conductive keratoplasty and laser thermal keratoplasty. Int Ophthalmol Clin. 2002. 42:99–106.
22. Ayoubi MG, Leccisotti A, Goodall EA, et al. Femtosecond laser in situ keratomileusis versus conductive keratoplasty to obtain monovision in patients with emmetropic presbyopia. J Cataract Refract Surg. 2010. 36:997–1002.
23. Esquenazi S, He J, Kim DB, et al. Wound-healing response and refractive regression after conductive keratoplasty. J Cataract Refract Surg. 2006. 32:480–486.
24. Guzowski M, Wang JJ, Rochtchina E, et al. Five-year refractive changes in an older population: the Blue Mountains Eye Study. Ophthalmology. 2003. 110:1364–1370.
25. Lee KE, Klein BE, Klein R. Changes in refractive error over a 5-year interval in the Beaver Dam Eye Study. Invest Ophthalmol Vis Sci. 1999. 40:1645–1649.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download