Abstract
Purpose
To investigate the regional characteristics and the factors that influence final visual acuity in corneal laceration and use the results for prevention and treatment of corneal laceration.
Methods
Sixty-eight patients who visited the Chosun University Medical Center from January 1, 2006 to December 31, 2010 were retrospectively surveyed. The incidence of corneal laceration, sex, age, monthly and seasonal distribution, cause, site and length of corneal laceration, secondary operation, complications, and ocular trauma score were reviewed statistically. In additional, the factors influencing visual prognosis were investigated.
Results
The incidence was more common in males (94.1%) and in the 6th-decade of life (29.4%). The corneal laceration was more common in the summer (38.2%) and in September (26.5%) and the most common cause was stone (39.7%) and metal (35.3%), respectively. The corneal laceration tended to occur at the corneal center. The most common first operation was primary closure (81.9%), and the secondary operation was most often performed due to a traumatic cataract (32.1%). The factors that significantly influenced the final visual acuity were initial visual acuity, length and site of laceration, and secondary operation.
Figures and Tables
 | Figure 3The ratio in different site of cornea. The corneal laceration tended to occur at the corneal center. |
 | Figure 4Final visual acuity and ocular trauma score. HM = hand motion; LP = light perception; NLP = no light perception; OTS = ocular trauma score. |
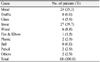
Table 3
Factors predicting visual outcome in 68 eyes with corneal laceration

NLP = no light perception; LP = light perception; HM = hand motion; S.T. = superotemporal; S.N. = superonasal; I.T. = inferotemporal; I.N. = inferonasal.
*A simplified categorical system for standardized assessment and visual prognosis in ocular injuries. It was calculated by assigning the following variables: initial visual acuity, globe rupture, endophthalmitis, perforating injury, retinal detachment, and a relative afferent pupillary defect.
References
1. Kuhn F, Maisiak R, Mann L, et al. The Ocular Trauma Score (OTS). Ophthalmol Clin North Am. 2002. 15:163–165.
2. Wurdermann . Injuries of the Eye. 1962. 2nd ed. St. Louis: CV Mosby;1–264. Part I.
3. Pieramici DJ, MacCumber MW, Humayun MU, et al. Open-globe injury. Update on types of injuries and visual results. Ophthalmology. 1996. 103:1798–1803.
4. Rhee HC, Chung SM, Rhea SW, Lee WC. Industrial ocular injary in St. Mary's industrial accident hospital. J Korean Ophthalmol Soc. 1989. 30:995–1001.
5. Edmund J. The prognosis of perforating eye injuries. Acta Ophthalmol (Copenh). 1968. 46:1165–1174.
6. Duke-Elder S. Injuries. System of Ophthalmology. 1972. Vol. 14. London: Henry Kimpton;574–576.
7. Ahn JW, Moon SH, Lee DH, Lee CY. Factors influencing final visual acuity after penetrating ocular injuries. J Korean Ophthalmol Soc. 1998. 39:2451–2458.
8. Han YS, Shyn KH. A statistical observation of the ocular injuries. J Korean Ophthalmol Soc. 2005. 46:117–124.
9. Song MH, Kim JW, Chung SK. The statistical observation of ocular injury. J Korean Ophthalmol Soc. 2009. 50:580–587.
10. Kim JH, Yang SJ, Kim DS, et al. Fourteen-year review of open globe injuries in an urban Korean population. J Trauma. 2007. 62:746–749.
11. Chung SM, Choi JY. A clinical study of penetrating ocular injuries. J Korean Ophthalmol Soc. 1997. 38:491–498.
12. Barr CC. Prognostic factors in corneoscleral lacerations. Arch Ophthalmol. 1983. 101:919–924.
13. Hutton WL, Fuller DG. Factors influencing final visual results in severely injured eyes. Am J Ophthalmol. 1984. 97:715–722.
14. Kim CW, Kim JM. Factors influencing the prognosis of corneoscleral laceration. J Korean Ophthalmol Soc. 1985. 26:311–319.
15. Sternberg P Jr, de Juan E Jr, Michels RG, Auer C. Multivariate analysis of prognostic factors in penetrating ocular injuries. Am J Ophthalmol. 1984. 98:467–472.
16. Kim JJ, Park BK, Lee SH, Oh SM. Ocular injuries, analytical view of 340 cases. J Korean Ophthalmol Soc. 1969. 10:27–31.
17. Kim SY, Park JM. A Clinical Observation of corneal laceration with traumatic cataract. J Korean Ophthalmol Soc. 1995. 36:1694–1699.
18. Yoo JH, Lee H, Lee J, et al. A statistical observation of ocular injuries and visual predictive value of ocular trauma score. J Korean Ophthalmol Soc. 2011. 52:1024–1029.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download