Abstract
Purpose
To evaluate the long-term prognosis and complications of laser epithelial keratomileusis (LASEK).
Methods
A retrospective study including 92 eyes of 46 myopic patients treated with LASEK from November 1999 to February 2003 was performed. Follow-up visits were at 3 months, 6 months, 1 year, and 8 years. Treated eyes were divided into 2 groups according to preoperative spherical equivalent (SE) : low and medium myopia (<-6.0 D), and high myopia (>-6.0 D). The main outcome measures were UCVA, BCVA, postoperative SE, efficacy index, safety index, predictability, and postoperative complications.
Results
Preoperative visual acuity was 1.24 ± 0.42 log MAR, and the average of SE was -5.28 ± 1.63 D. Postoperative visual acuity log MAR was significantly improved compared to preoperative visual acuity, and the average of visual acuity was 0.12 ± 0.13 log MAR. The percentage of eyes within ± 1.0 D of emmetropia 8 years after having LASEK was 69.5% in the mild and moderate myopia group, and 63.6% in the high myopia group. There was no significant difference of safety index, efficacy index or complications between the 2 groups at 1 month, 3 months, 1 year, and 8 years. Safety index was maintained over 0.9 and efficacy index was larger than 0.8. There were no other complications during the observation period.
Figures and Tables
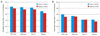 | Figure 1(A) Bar graph representing the percentage of eyes within ± 1.0 D of emmetropia (in aspect of spherical equivalent) at 8 years after LASEK. (B) The percentage of eyes within ± 0.5 D of emmetropia. |
References
1. Camellin M. Laser epithelial keratomileusis for myopia. J Refract Surg. 2003. 19:666–670.
2. Kim SY, Sah WJ, Lim YW, Hahn TW. Twenty percent alcohol toxicity on rabbit corneal epithelial cells: electron microscopic study. Cornea. 2002. 21:388–392.
3. Carones F, Fiore T, Brancato R. Mechanical vs. alcohol epithelial removal during photorefractive keratectomy. J Refract Surg. 1999. 15:556–562.
4. Kanitkar KD, Camp J, Humble H, et al. Pain after epithelial removal by ethanol-assisted mechanical versus transepithelial excimer laser debridement. J Refract Surg. 2000. 16:519–522.
5. Stein HA, Stein RM, Price C, Salim GA. Alcohol removal of the epithelium for excimer laser ablation: outcomes analysis. J Cataract Refract Surg. 1997. 23:1160–1163.
6. Scerrati E. Laser in situ keratomileusis vs. laser epithelial keratomileusis (LASIK vs. LASEK). J Refract Surg. 2001. 17:2 Suppl. S219–S221.
7. Anderson NJ, Beran RF, Schneider TL. Epi-LASEK for the correction of myopia and myopic astigmatism. J Cataract Refract Surg. 2002. 28:1343–1347.
8. Litwak S, Zadok D, Garcia-de Quevedo V, et al. Laser-assisted subepithelial keratectomy versus photorefractive keratectomy for the correction of myopia. A prospective comparative study. J Cataract Refract Surg. 2002. 28:1330–1333.
9. Dastjerdi MH, Soong HK. LASEK (laser subepithelial keratomileusis). Curr Opin Ophthalmol. 2002. 13:261–263.
10. Kim DH, Kim JH. Two year clinical results of LASEK (laser epithelial keratomileusis) for correcting myopia. J Korean Ophthalmol Soc. 2003. 44:2473–2479.
11. Kong HY, Ko IH, Lee JB. Comparison of laser epithelial keratomileusis(LASEK) in one eye and photorefractive keratectomy(PRK) in other eye for low to moderate myopia. J Korean Ophthalmol Soc. 2001. 42:825–831.
12. Alió JL, Muftuoglu O, Ortiz D, et al. Ten-year follow-up of photorefractive keratectomy for myopia of less than -6 diopters. Am J Ophthalmol. 2008. 145:29–36.
13. Alió JL, Muftuoglu O, Ortiz D, et al. Ten-year follow-up of photorefractive keratectomy for myopia of more than -6 diopters. Am J Ophthalmol. 2008. 145:37–45.
14. Pietilä J, Mäkinen P, Pajari T, et al. Eight-year follow-up of photorefractive keratectomy for myopia. J Refract Surg. 2004. 20:110–115.
15. Kinge B, Midelfart A, Jacobsen G, Rystad J. Biometric changes in the eyes of Norwegian university students--a three-year longitudinal study. Acta Ophthalmol Scand. 1999. 77:648–652.
16. Taneri S, Zieske JD, Azar DT. Evolution, techniques, clinical outcomes, and pathophysiology of LASEK: review of the literature. Surv Ophthalmol. 2004. 49:576–602.




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download