Abstract
Purpose
To compare long-term outcomes of penetrating keratoplasty in treating macular corneal dystrophy, transforming growth factor beta induced (TGFBI) dystrophy, and Fuchs' dystrophy.
Methods
The present retrospective study describes the postoperative results of 123 eyes in 70 patients; 53 eyes with macular corneal dystrophy, 20 eyes with TGFBI dystrophy, and 50 eyes with Fuchs' dystrophy. All patients received penetrating keratoplasty. The outcome measures included recurrence rate, graft rejection, graft survival rate and corneal endothelial density and other complications.
Results
As compared with the other groups, TGFBI dystrophy had the highest recurrence rate (p-value < 0.0001). Fuchs' dystrophy had the lowest graft survival rate (p-value = 0.03). Corneal endothelial cell density was lowest in Fuchs' dystrophy 10 years postoperatively (p-value = 0.0006), but there was no significant difference in corneal endothelial cell density between the 3 groups 1 and 5 years postoperatively. There was no significant difference between the 3 groups in other complications such as graft rejection, secondary glaucoma and persistent epithelial defect (p-value = 0.809, p-value = 0.584, p-value = 0.972, respectively).
Figures and Tables
Figure 1
Kaplan-Meier graph showing overall recurrence-free survival rate of penetrating keratoplasty in treating three corneal dystrophy groups. As compared with the other groups, TGFBI corneal dystrophy group had the highest recurrence rate (p-value < 0.0001).

Figure 2
Kaplan-Meier graph showing overall graft survival rate of penetrating keratoplasty in treating three corneal dystrophy groups. Fuchs' dystrophy had the lowest graft survival rate (p-value = 0.03).

Figure 3
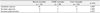
Bar graph showing changes of corneal endothelial cell density of penetrating keratoplasty in treating three corneal dystrophy groups. Corneal endothelial cell density was lowest in Fuchs' dystrophy 10 years postoperatively (*p-value = 0.032), but there was no significant difference in corneal endothelial cell density between the 3 groups 1 and 5 years postoperatively.

References
1. Bron AJ, Aldave A, Akhtar S, et al. Tasman W, Jaeger EA, editors. Inherited dystrophies and developmental anomalies of the cornea. Duane's Ophthalmology. 2008. 2009 ed. Philadelphia: Lippincott Williams & Wilkins.
2. Jones ST, Zimmerman LE. Histopathologic differentiation of granular, macular and lattice dystrophies of the cornea. Am J Ophthalmol. 1961. 51:394–410.
3. Jones ST, Zimmerman LE. Macular dystrophy of the cornea (Groenouw type II); clinicopathologic report of two cases with comments concerning its differential diagnosis from lattice dystrophy (Biber-Haab-Dimmer). Am J Ophthalmol. 1959. 47(1 Part 1):1–16.
4. Weiss JS, Møller HU, Lisch W, et al. The IC3D classification of the corneal dystrophies. Cornea. 2008. 27:Suppl 2. S1–S83.
5. Møller HU, Weiss JS. IC3D classification of corneal dystrophies. Dev Ophthalmol. 2011. 48:1–8.
6. Al-Swailem SA, Al-Rajhi AA, Wagoner MD. Penetrating keratoplasty for macular corneal dystrophy. Ophthalmology. 2005. 112:220–224.
7. Akama TO, Nishida K, Nakayama J, et al. Macular corneal dystrophy type I and type II are caused by distinct mutations in a new sulphotransferase gene. Nat Genet. 2000. 26:237–241.
8. Malbran ES. Macular corneal dystrophy in Saudi Arabia: a study of 56 cases and recognition of a new immunophenotype. Am J Ophthalmol. 1998. 125:417–418.
9. Jonasson F, Oshima E, Thonar EJ, et al. Macular corneal dystrophy in Iceland. A clinical, genealogic, and immunohistochemical study of 28 patients. Ophthalmology. 1996. 103:1111–1117.
10. Cho YA, Kim MH, Oh JS. A case of macular dystrophy of the cornea. J Korean Ophthalmol Soc. 1976. 17:217–221.
11. Kim IS, Myong YW. Cases of macular corneal dystrophy with a family history. J Korean Ophthalmol Soc. 1995. 36:874–878.
12. Skonier J, Neubauer M, Madisen L, et al. cDNA cloning and sequence analysis of beta ig-h3, a novel gene induced in a human adenocarcinoma cell line after treatment with transforming growth factor-beta. DNA Cell Biol. 1992. 11:511–522.
13. Zhang T, Yan N, Yu W, et al. Molecular genetics of Chinese families with TGFBI corneal dystrophies. Mol Vis. 2011. 17:380–387.
14. Escribano J, Hernando N, Ghosh S, et al. cDNA from human ocular ciliary epithelium homologous to beta ig-h3 is preferentially expressed as an extracellular protein in the corneal epithelium. J Cell Physiol. 1994. 160:511–521.
15. El Kochairi I, Letovanec I, Uffer S, et al. Systemic investigation of keratoepithelin deposits in TGFBI/BIGH3-related corneal dystrophy. Mol Vis. 2006. 12:461–466.
16. Yao YF, Jin YQ, Zhang B, et al. Recurrence of lattice corneal dystrophy caused by incomplete removal of stroma after deep lamellar keratoplasty. Cornea. 2006. 25:10 Suppl 1. S41–S46.
17. Meisler DM, Fine M. Recurrence of the clinical signs of lattice corneal dystrophy (type I) in corneal transplants. Am J Ophthalmol. 1984. 97:210–214.
18. Lyons CJ, McCartney AC, Kirkness CM, et al. Granular corneal dystrophy. Visual results and pattern of recurrence after lamellar or penetrating keratoplasty. Ophthalmology. 1994. 101:1812–1817.
19. Adamis AP, Filatov V, Tripathi BJ, Tripathi RC. Fuchs' endothelial dystrophy of the cornea. Surv Ophthalmol. 1993. 38:149–168.
20. Pineros O, Cohen EJ, Rapuano CJ, Laibson PR. Long-term results after penetrating keratoplasty for Fuchs' endothelial dystrophy. Arch Ophthalmol. 1996. 114:15–18.
21. Happ DM, Lewis DA, Eng KH, et al. Postoperative visual acuity in patients with fuchs dystrophy undergoing descemet membrane-stripping automated endothelial keratoplasty: correlation with the severity of histologic changes. Arch Ophthalmol. 2012. 130:33–38.
22. Lee HS, Kim MS. Influential factors on the survival of endothelial cells after penetrating keratoplasty. Eur J Ophthalmol. 2009. 19:930–935.
23. Langenbucher A, Seitz B, Nguyen NX, Naumann GO. Corneal endothelial cell loss after nonmechanical penetrating keratoplasty depends on diagnosis: a regression analysis. Graefes Arch Clin Exp Ophthalmol. 2002. 240:387–392.
24. Yellore VS, Rayner SA, Aldave AJ. TGFB1-induced extracellular expression of TGFBIp and inhibition of TGFBIp expression by RNA interference in a human corneal epithelial cell line. Invest Ophthalmol Vis Sci. 2011. 52:757–763.
25. Aldave AJ, Sonmez B, Forstot SL, et al. A clinical and histopathologic examination of accelerated TGFBIp deposition after LASIK in combined granular-lattice corneal dystrophy. Am J Ophthalmol. 2007. 143:416–419.
26. Kannabiran C, Klintworth GK. TGFBI gene mutations in corneal dystrophies. Hum Mutat. 2006. 27:615–625.
27. Klintworth GK, Reed J, Stainer GA, Binder PS. Recurrence of macular corneal dystrophy within grafts. Am J Ophthalmol. 1983. 95:60–72.
28. Akova YA, Kirkness CM, McCartney AC, et al. Recurrent macular corneal dystrophy following penetrating keratoplasty. Eye (Lond). 1990. 4(Pt 5):698–705.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download