Abstract
Purpose
To describe the clinical manifestations and magnetic resonance imaging (MRI) characteristics of idiopathic optic perineuritis patients in Korea.
Methods
A retrospective chart review of 5 patients (6 eyes) with idiopathic optic perineuritis and 7 patients (7 eyes) with optic neuritis was performed.
Results
The mean age of the 5 patients with idiopathic optic perineuritis was 59 years, and the mean age of the 7 patients with optic neuritis was 31.1 years. A relative afferent papillary defect (RAPD) was present in 4 eyes with idiopathic optic perineuritis, and in all 7 eyes with optic neuritis. All six eyes with idiopathic optic perineuritis showed relatively severe optic disc swelling, and 6 eyes with optic neuritis showed mild optic disc swelling. MRI demonstrated optic nerve sheath enhancement in all patients with idiopathic optic perineuritis and optic nerve enhancement in six patients with optic neuritis.
Conclusions
On MRI, compared with optic neuritis, idiopathic optic perineuritis had a higher onset age, relatively severe optic disc swelling, and optic nerve sheath enhancement. Because idiopathic optic perineuritis is known to have different treatment strategies and prognosis compared with optic neuritis, differential diagnosis is crucial. The clinical manifestations and MRI characteristics of idiopathic optic perineuritis in the present study will help in the diagnosis of Korean patients.
Figures and Tables
Figure 1
(A) Fundus photography of 66-year-old male patient (Case 4) with idiopathic optic perineuritis shows grade IV optic disc edema in his right eye. He presented with known optic disc edema of 7 weeks in the right eye. (B) Fundus photography after oral steroid treatment.
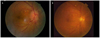
Figure 2
Magnetic resonance imaging scan of the orbit with contrast infusion and fat suppression in case 4 with idiopathic optic perineuritis. Axial and coronal view show enhancement of the right optic nerve sheath and streakiness of the surrounding orbital fat.
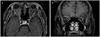
Table 1
Clinical manifestations of idiopathic optic perineuritis

VA = visual acuity by Snellen visual acuity chart; VF = visual field; RAPD, relative afferent pupillary defect; MRI = magnetic resonance imaging; ST = superotemporal; LU = log unit; ONS = optic nerve sheath; CF = counting finger; ON = optic nerve; EOM = extraocular muscle.
*This patient experienced idiopathic optic perineuritis in the right eye at first. However, at 5 months after resolution, idiopathic optic perineuritis occurred in the left eye.
References
1. Kennerdell JS, Dresner SC. The nonspecific orbital inflammatory syndromes. Surv Ophthalmol. 1984. 29:93–103.
2. Nassani S, Cocito L, Arcuri T, Favale E. Orbital pseudotumor as a presenting sign of temporal arteritis. Clin Exp Rheumatol. 1995. 13:367–369.
3. Oh HG, Yang KI. A case of optic perineuritis associated with seronegative neurosyphilis. J Korean Geriatr Soc. 2007. 11:98–100.
4. Purvin V, Kawasaki A, Jacobson DM. Optic perineuritis: clinical and radiographic features. Arch Ophthalmol. 2001. 119:1299–1306.
5. Thompson HS, Corbett JJ, Cox TA. How to measure the relative afferent pupillary defect. Surv Ophthalmol. 1981. 26:39–42.
6. Singh AD, Kivelä T. The collaborative ocular melanoma study. Ophthalmol Clin North Am. 2005. 18:129–142.
7. Margo CE. The Collaborative Ocular Melanoma Study: an overview. Cancer Control. 2004. 11:304–309.
8. Frisén L. Swelling of the optic nerve head: a staging scheme. J Neurol Neurosurg Psychiatry. 1982. 45:13–18.
9. Edmunds W, Lawford JB. Examination of optic nerve from cases of amblyopia in diabetes. Trans Ophthalmol Soc UK. 1883. 3:160–162.
10. Fay AM, Kane SA, Kazim M, et al. Magnetic resonance imaging of optic perineuritis. J Neuroophthalmol. 1997. 17:247–249.
11. Hickman SJ, Miszkiel KA, Plant GT, Miller DH. The optic nerve sheath on MRI in acute optic neuritis. Neuroradiology. 2005. 47:51–55.
12. Beck RW, Cleary PA. Optic neuritis treatment trial. One-year follow-up results. Arch Ophthalmol. 1993. 111:773–775.
13. Beck RW, Cleary PA, Backlund JC. The course of visual recovery after optic neuritis. Experience of the Optic Neuritis Treatment Trial. Ophthalmology. 1994. 101:1771–1778.
14. Ahn BC, Kim HS, Ahn HS. Clinical profile of the optic neuritis in Korea. J Korean Ophthalmol Soc. 1997. 38:1827–1833.
15. Lee YJ, Chang BL. Clinical manifestations of optic neuritis. J Korean Ophthalmol Soc. 1997. 38:1969–1974.
16. Yang DW, Lee SH. Clinical characteristics of optic neuritis according to the presence of abnormal MRI lesions. J Korean Ophthalmol Soc. 2004. 45:273–280.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download