Abstract
Purpose
To determine predictable factors of postoperative pain and cut-off values following LASEK eye surgery.
Methods
Thirty-three eyes of 17 patients who underwent LASEK from May to December 2008 were reviewed. For evaluation of predictive factors, patients' anxiety level was converted to APAIS, HADS, STAI, and VAS preoperatively. Substance P and prostaglandin E2 levels in tears, blood pressure, heart rate, and history of any previous surgery were determined before the procedure. Thirty minutes and 1 day after LASEK, the subjective degree of pain was scored.
Results
Patients with high Amsterdam preoperative anxiety scale (APAIS) and Visual analogue scale (VAS) scores showed more postoperative pain (p=0.04, p<0.001). Higher substance P and prostaglandin E2 levels were significantly related with more severe pain after LASEK (p<0.001, p<0.001). Postoperative pain increased significantly, according to cut-off values (p<0.05), APAIS and VAS scores greater than 6, substance P greater than 631.84 pg/ml, and prostaglandin E2 greater than 783.90 pg/ml.
Figures and Tables
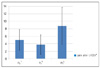 | Figure 2Mean postoperative pain following LASEK.
*Postoperative pain measurement by VAS (Visual Analogue Scale); †P0 = pain at 30 minutes postoperatively; ‡P1 = pain at 1 day postoperatively; §PT = total pain (P0+P1).
|
Table 1
Predictive factors of postoperative pain following LASEK

*SBP = systolic blood pressure; †DBP = diastolic blood pressure; ‡HR = heart rate; §APAIS = Amsterdam preoperative anxiety information scale; ∥HADS = hospital anxiety anxiety depression scale; ¶STAI = state-trait anxiety scale; #VAS = visual analogue scale; **SP = substance P; ††PGE2 = prostaglandin E2.
References
1. Trokel SL, Srinivasan R, Braren B. Excimer laser surgery of the cornea. Am J Ophthalmol. 1983. 96:710–715.
2. Gartry DS, Kerr Muir MG, Marshall J. Excimer laser photorefractive keratectomy. 18-month follow-up. Ophthalmology. 1992. 99:1209–1219.
3. Spigelman AV. Complications of LASIK. J Refract Surg. 2001. 17:475.
4. Pallikaris IG, Kymionis GD, Astyrakakis NI. Corneal ectasia induced by laser in situ keratomileusis. J Cataract Refract Surg. 2001. 27:1796–1802.
5. Carones F, Fiore T, Brancato R. Mechanical vs. alcohol epithelial removal during photorefractive keratectomy. J Refract Surg. 1999. 15:556–562.
6. Hersh PS, Brint SF, Maloney RK, et al. Photorefractive keratectomy versus laser in situ keratomileusis for moderate to high myopia. A randomized prospective study. Ophthalmology. 1998. 105:1512–1522. discussion 22-3.
7. Hersh PS, Steinert RF, Brint SF. Summit PRK-LASIK Study Group. Photorefractive keratectomy versus laser in situ keratomileusis: comparison of optical side effects. Ophthalmology. 2000. 107:925–933.
8. O'Doherty M, Kirwan C, O'Keeffe M, O'Doherty J. Postoperative pain following epi-LASIK, LASEK, and PRK for myopia. J Refract Surg. 2007. 23:133–138.
9. Moerman N, van Dam FS, Muller MJ, Oosting H. The Amsterdam Preoperative Anxiety and Information Scale (APAIS). Anesth Analg. 1996. 82:445–451.
10. Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983. 67:361–370.
11. Spielberger CD, Vagg PR. Psychometric properties of the STAI: a reply to Ramanaiah, Franzen, and Schill. J Pers Assess. 1984. 48:95–97.
12. Chung SK, et al. Comparison in Pain between Photorefractive and Laser In Situ Epithelial Keratomileusis during Intraoperative and Postoperative Period. J Korean Ophthalmol Soc. 2001. 42:563–568.
13. Kalkman CJ, Visser K, Moen J, et al. Preoperative prediction of severe postoperative pain. Pain. 2003. 105:415–423.
14. Shin WJ, et al. The Validity of Amsterdam Preoperative Anxiety Information Scale in the Assessment of the Preoperative Anxiety. J Korean Anesthesiol. 1998. 37:179–187.
15. Nisbet HI, Norris W. Objective Measurement of Sedation. Ii. A Simple Scoring System. Br J Anaesth. 1963. 35:618–623.
16. Beechey AP, Eltringham RJ, Studd C. Temazepam as premedication in day surgery. Anaesthesia. 1981. 36:10–15.
17. Poulton EC. Models for biases in judging sensory magnitude. Psychol Bull. 1979. 86:777–803.
18. Phillips AF, Szerenyi K, Campos M, et al. Arachidonic acid metabolites after excimer laser corneal surgery. Arch Ophthalmol. 1993. 111:1273–1278.
19. Yamada M, Ogata M, Kawai M, et al. Substance P and its metabolites in normal human tears. Invest Ophthalmol Vis Sci. 2002. 43:2622–2625.
20. Gluud BS, Jensen OL, Krogh E. Prostaglandin E2 in tears. Acta Ophthalmol Suppl. 1985. 173:28–29.
21. Yamada M, Ogata M, Kawai M, et al. Substance P in human tears. Cornea. 2003. 22:S48–S54.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download