Abstract
Purpose
To predict the accuracy of preoperative refractive error measurement methods in wavefront-guided laser-assisted subepithelial keratectomy (LASEK) surgery and to formulate a nomogram for satisfactory surgical results.
Methods
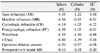
The medical records of 30 patients (57 eyes) who had undergone wavefront-guided LASEK were reviewed. The ideal surgical ablation amount was defined as the sum of the real surgical ablation amount and the remaining refractive errors. Comparison between the ideal surgical ablation amount and preoperative refractive errors was made using autorefraction, manifest refraction, cycloplegic refraction, postcycloplegic refraction, wavescan, and iTrace aberrometer measurements.
Results
The refractive errors measured by the postcycloplegic refraction showed the closest relation with the ideal surgical amount, and the nomogram based on this refraction correlated statistically significantly with the ideal surgical ablation amount. The refractive error using the wavescan also showed more accurate refractive measurements than the autorefractor and iTrace aberrometer.
Conclusions
Accurate manifest refraction immediately before surgery is the most important in determining the ablation amount. Additionally, the refractive errors measured with the wavescan, which is an aberrometer used for wavefront-guided LASEK, showed a minimal amount of errors. After reviewing the results, the nomogram based on these 2 methods can be concluded to possibly contribute to an increase in the accuracy of surgery.
Figures and Tables
 | Figure 1Correlation and correlation coefficient between postcycloplegic refractive error and ideal surgical ablation amount. (A)Sphere. (B) Cylinder. D=diopters; PC=postcycloplegic refraction; sph=sphere; cyl=cylinder. |
 | Figure 2The differences between residual spherical refractive errors after ablation and preoperative refractive errors using various methods. These graphs are showing the distribution of the residual spherical refractive errors for each of all patients. The residual refractive error is defined as the value of the amount of the ideal surgical ablation minus the preoperative refractive errors measuring with various methods. D=diopters; AR=autorefraction; MR=manifest refraction; CR=cycloplegic refraction; PC=postcycloplegic refraction. |
 | Figure 3The differences between residual cylindrical refractive error after ablation and preoperative refractive errors using various methods. These graphs are showing the distribution of the residual cylindrical refractive errors for each of all patients. The residual refractive error is defined as the value of the amount of the ideal surgical ablation minus the preoperative refractive errors measuring with various methods. D=diopters; AR=autorefraction; MR=manifest refraction; CR=cycloplegic refraction; PC=postcycloplegic refraction. |
References
1. Doane JF, Slade SG. An introduction to wavefront-guided refractive surgery. Int Ophthalmol Clin. 2003. 43:101–117.
2. Charman WN. Wavefront aberration of the eye: a review. Optom Vis Sci. 1991. 68:574–583.
3. Wang L, Wang N, Koch DD. Evaluation of refractive error measurements of the wavescan wavefront system and the Tracey wavefront aberrometer. J Cataract Refract Surg. 2003. 29:970–979.
4. Reinstein DZ, Archer TJ, Couch D. Accuracy of the WASCA aberrometer refraction compared to manifest refraction in myopia. J Refract Surg. 2006. 22:268–274.
5. Park SJ, Wee WR, Lee JH, Kim MK. Comparison of wavescan aberrometer refraction to subjective manifest refraction and autorefractor. J Korean Ophthamol Soc. 2009. 50:684–690.
6. Elliott M, Simpson T, Richter D, Fonn D. Repeatability and accuracy of automated refraction: a comparison of the Nikon NRK-8000, the Nidek AR-1000, and subjective refraction. Optom Vis Sci. 1997. 74:434–438.
7. Kinge B, Midelfart A, Jacobssen G. Clinical evaluation of the Allergan Humphrey 500 autorefractor and the Nidek AR-1000 autorefractor. Br J Ophthalmol. 1996. 80:35–39.
8. Mallen EA, Wolffsohn JS, Gilmartin B, Tsujimura S. Clinical evaluation of the Shin-Nippon SRW-5000 autorefractor in adults. Ophthalmic Physiol Opt. 2001. 21:101–107.
9. Gwiazda J, Weber C. Comparison of spherical equivalent refraction and astigmatism measured with three different models of autorefractors. Optom Vis Sci. 2004. 81:56–61.
10. Nayak BK, Ghose S, Singh JP. A comparison of cycloplegic and manifest refractions on the NR-1000F (an objective auto refractometer). Br J Ophthalmol. 1987. 71:73–75.
11. Ghose S, Nayak BK, Singh JP. Critical evaluation of the NR-1000F auto refractometer. Br J Ophthalmol. 1986. 70:221–226.
12. Wesemann W, Rassow B. Automatic infrared refractors-comparative study. Am J Optom Physiol Opt. 1987. 64:627–638.
13. Mcbrien NA, Millodot M. Clinical evaluation of the Canon Autoref R-1. Am J Optom Physiol Opt. 1985. 62:786–792.
14. Raj PS, Villada JR, Lewis AE, et al. Comparative evaluation of the Allergan Humphrey 570 and Canon RK-1 autorefractors. I. Objective refraction in normal subjects. Eye. 1992. 6:284–286.
15. Jorge J, Queiros A, Gonzalez-Meijome J, et al. The influence of cycloplegia in objective refraction. Ophthalmic Physiol Opt. 2005. 25:340–345.
16. Thibos LN. Principles of Hartmann-Shack aberrometry. J Refract Surg. 2000. 16:S563–S565.
17. Liang J, Grimm B, Goelz S, Bille JF. Objective measurement of wave aberrations of the human eye with the use of a Hartmann-Shack wave-front sensor. J Opt Soc Am A Opt Image Sci Vis. 1994. 11:1949–1957.
18. Lee SM, Lee MJ, Kim MK, et al. Comparison of changes in Higher-order aberrations between conventional and wavefront-guided LASEK. J Korean Ophthalmol Soc. 2007. 48:1028–1035.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download