| Korean J Gastroenterol. 2016 Jan;67(1):22-27. Korean. Published online Jan 26, 2016. https://doi.org/10.4166/kjg.2016.67.1.22 | |
| Copyright © 2016 The Korean Society of Gastroenterology | |
|
Sun Hee Park,
Young Woon Chang, | |
| Department of Internal Medicine, Kyung Hee University Hospital, Kyung Hee University College of Medicine, Seoul, Korea. | |
|
1Maeil Innovation Center, Maeil Daires Co., Ltd., Pyeongtaek, Korea. | |
| Received October 26, 2015; Revised December 31, 2015; Accepted January 05, 2016. | |
|
This is an open access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by- | |
|
Abstract
| |
|
Background/Aims
Lactose-free milk (LFM) is available for nutrient supply for those with lactose intolerance (LI). However, there are no consistent results of the efficacy of LFM in LI subjects. We aimed to examine the changes of gastrointestinal (GI) symptoms and hydrogen breath test (HBT) values after ingestion of lactose contained milk (LCM) vs. LFM.
Methods
From May 2015 to September 2015, thirty-five healthy adults with history of LCM-induced GI symptoms were recruited at a tertiary hospital. For the diagnosis of LI, HBT with LCM 550 mL (lactose 25 g) was performed every 20 minutes for 3 hours. The test was defined as "positive" when H2 peak exceeded 20 ppm above baseline values (ΔH2>20 ppm). When the subjects are diagnosed as LI, the second HBT using LFM 550 mL (lactose 0 g) was performed 7 days later. Subjects were asked to complete a questionnaire about the occurrence and severity of GI symptoms.
Results
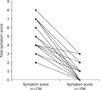
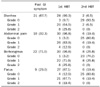
Among a total of 35 subjects, 31 were diagnosed with LI at first visit, and their LCM-related symptoms were abdominal pain (98.6%), borborygmus (96.8%), diarrhea (90.3%), and flatus (87.1%). The ΔH2 value in subjects taking LCM (103.7±66.3 ppm) significantly decreased to 6.3±4.9 ppm after ingesting LFM (p<0.0001). There were also significant reduction in total symptom scores and the severity of each symptom when LCM was changed to LFM (p<0.0001).
Conclusions
This is the first report that LFM reduce LCM-related GI symptoms and H2 production in Korean adults. LFM can be an effective alternative for LCM in adults with LI. |
|
Keywords: Breath tests; Hydrogen; Lactose intolerance |
|
|
Figures
|
|
|
|
|
Tables
|
|
|
Notes
|
Financial support:This research was supported by research fund from Maeil Innovation Center, Maeil Daires Co., Ltd.
Conflict of interest:None.
|
References
|
| 1. | Rusynyk RA, Still CD. Lactose intolerance. J Am Osteopath Assoc 2001;101 4 Suppl Pt 1:S10–S12. |
| 2. | Jellema P, Schellevis FG, van der Windt DA, Kneepkens CM, van der Horst HE. Lactose malabsorption and intolerance: a systematic review on the diagnostic value of gastrointestinal symptoms and self-reported milk intolerance. QJM 2010;103:555–572. |
| 3. | Swagerty DL Jr, Walling AD, Klein RM. Lactose intolerance. Am Fam Physician 2002;65:1845–1850. |
| 4. | Chang YW, Park CG, Bang IS, Chang R, Min YI. A study of lactose intolerance using breath hydrogen test in Korean healthy adults. Korean J Intern Med 1986;30:643–649. |
| 5. | Levitt M, Wilt T, Shaukat A. Clinical implications of lactose malabsorption versus lactose intolerance. J Clin Gastroenterol 2013;47:471–480. |
| 6. | Law D, Conklin J, Pimentel M. Lactose intolerance and the role of the lactose breath test. Am J Gastroenterol 2010;105:1726–1728. |
| 7. | Matthews SB, Waud JP, Roberts AG, Campbell AK. Systemic lactose intolerance: a new perspective on an old problem. Postgrad Med J 2005;81:167–173. |
| 8. | Tolliver BA, Jackson MS, Jackson KL, Barnett ED, Chastang JF, DiPalma JA. Does lactose maldigestion really play a role in the irritable bowel? J Clin Gastroenterol 1996;23:15–17. |
| 9. | Romagnuolo J, Schiller D, Bailey RJ. Using breath tests wisely in a gastroenterology practice: an evidence-based review of indications and pitfalls in interpretation. Am J Gastroenterol 2002;97:1113–1126. |
| 10. | Suchy FJ, Brannon PM, Carpenter TO, et al. NIH consensus development conference statement: lactose intolerance and health. NIH Consens State Sci Statements 2010;27:1–27. |
| 11. | Montalto M, Curigliano V, Santoro L, et al. Management and treatment of lactose malabsorption. World J Gastroenterol 2006;12:187–191. |
| 12. | Hermans MM, Brummer RJ, Ruijgers AM, Stockbrügger RW. The relationship between lactose tolerance test results and symptoms of lactose intolerance. Am J Gastroenterol 1997;92:981–984. |
| 13. | Newcomer AD, McGill DB, Thomas PJ, Hofmann AF. Prospective comparison of indirect methods for detecting lactase deficiency. N Engl J Med 1975;293:1232–1236. |
| 14. | Park MJ, Lee JH, Kim KA, et al. The changes in the breath hydrogen concentration after the ingestion of Bifidobacterium breve KY-16 in the lactose malabsorbers. Korean J Gastroenterol 1999;34:741–748. |
| 15. | de Vrese M, Laue C, Offick B, et al. A combination of acid lactase from Aspergillus oryzae and yogurt bacteria improves lactose digestion in lactose maldigesters synergistically: a randomized, controlled, double-blind cross-over trial. Clin Nutr 2015;34:394–399. |
| 16. | Shaukat A, Levitt MD, Taylor BC, et al. Systematic review: effective management strategies for lactose intolerance. Ann Intern Med 2010;152:797–803. |
| 17. | Montalto M, Nucera G, Santoro L, et al. Effect of exogenous beta-galactosidase in patients with lactose malabsorption and intolerance: a crossover double-blind placebo-controlled study. Eur J Clin Nutr 2005;59:489–493. |
| 18. | Shaw AD, Davies GJ. Lactose intolerance: problems in diagnosis and treatment. J Clin Gastroenterol 1999;28:208–216. |
| 19. | Christl SU, Murgatroyd PR, Gibson GR, Cummings JH. Production, metabolism, and excretion of hydrogen in the large intestine. Gastroenterology 1992;102:1269–1277. |
| 20. | La Brooy SJ, Male PJ, Beavis AK, Misiewicz JJ. Assessment of the reproducibility of the lactulose H2 breath test as a measure of mouth to caecum transit time. Gut 1983;24:893–896. |
| 21. | Dainese R, Casellas F, Mariné-Barjoan E, et al. Perception of lactose intolerance in irritable bowel syndrome patients. Eur J Gastroenterol Hepatol 2014;26:1167–1175. |
| 22. | Goldstein R, Braverman D, Stankiewicz H. Carbohydrate malabsorption and the effect of dietary restriction on symptoms of irritable bowel syndrome and functional bowel complaints. Isr Med Assoc J 2000;2:583–587. |
| 23. | Pimentel M, Chow EJ, Lin HC. Normalization of lactulose breath testing correlates with symptom improvement in irritable bowel syndrome: a double-blind, randomized, placebo-controlled study. Am J Gastroenterol 2003;98:412–419. |
| 24. | Parker TJ, Woolner JT, Prevost AT, Tuffnell Q, Shorthouse M, Hunter JO. Irritable bowel syndrome: is the search for lactose intolerance justified? Eur J Gastroenterol Hepatol 2001;13:219–225. |
| 25. | Kim BG, Kim SM, Kim YS, et al. Sucrase to lactase activities ratio in duodenal mucosa as a diagnostic method of lactase deficiency. Korean J Gastroenterol 1997;29:175–181. |




 ePub
ePub Citation
Citation Print
Print