Abstract
Portal annular pancreas is one of the pancreatic fusion anomalies in which the uncinate process of the pancreas extends to fuse with the dorsal pancreas by encircling the portal vein or superior mesenteric vein. We report two consecutive patients with portal annular pancreas. The first case is a 71-year-old male patient who underwent a pancreaticoduodenectomy for intraductal papillary mucinous neoplasm in the head of pancreas. His preoperative computed tomography scan showed the suprasplenic type portal annular pancreas. The second case is a 74-year-old female patient who underwent a laparoscopic anterior radical antegrade modular pancreatosplenectomy (RAMPS) for pancreatic body cancer. In operative finding, portal confluence (superior mesenteric vein-splenic vein-portal vein) was encased with the uncinate process of pancreas in both cases. Therefore, they required pancreatic division at the pancreatic neck portion twice. During the postoperative period, grade B and A, respectively, postoperative pancreatic fistulas occurred and were controlled by conservative management. Surgeons need to know about this rare pancreatic condition prior to surgical intervention to avoid complications, and to provide patients with well-designed, case-specific pancreatic surgery.
Portal annular pancreas is one of the pancreatic fusion anomalies in which the uncinate process of the pancreas extends to fuse with the dorsal pancreas by surrounding the portal vein (PV) or superior mesenteric vein (SMV). It is more common in the porcine pancreas (Fig. 1),1 and is very rare in human. From a pancreatic surgeons' view point, a portal annular pancreas may influence the surgical procedure when dividing the neck of the pancreas, and can be potentially associated with postoperative pancreatic fistula because there are two pancreatic cut surfaces to manage when the pancreas needs to be divided at the level of the pancreatic neck portion. Here we present two consecutive patients with portal annular pancreas who underwent pancreaticoduodenectomy and subtotal distal pancreatectomy, respectively, and we discuss the clinical impact of this rare anomaly in certain types of pancreatectomy.
A 71-year-old male patient presented with diarrhea for 6 months. Under physical examination, there was no specific finding. A routine chemistry test showed mild elevation of serum amylase (203 U/L; reference range, 30-115 U/L) and lipase (66 U/L; reference range, 5-60 U/L). An abdominal CT scan revealed intraductal papillary mucinous neoplasm (IPMN) in the head of the pancreas, and portal annular pancreas was incidentally noted (Fig. 2A). There was no definite solid portion in the cystic mass, but diffuse soft tissue infiltration was identified around superior mesenteric artery and celiac axis with suspicious invasive nature (Fig. 2A picture in picture). MRCP demonstrated the branch duct type IPMN of 3.8 cm in diameter. Serum CA 19-9 level was elevated (85.6 U/mL; reference range, 0.0-37.0). Therefore, the patient underwent pylorus-preserving pancreaticoduodenectomy. Suprasplenic vein type portal annular pancreas was indentified. After careful dissection of the pancreatic neck portion, the pancreatic neck was first divided. Then, the uncinate process of pancreas surrounding the PV was divided by endo-GIA for pancreatic head resection (Fig. 2B-D). The usual type of pancreaticojejunostomy, hepaticojejunostomy, and duodenojejunostomy was performed. Postoperative pancreatic fistula (grade B) occurred, but was controlled by conservative management. He was able to go home on 49th postoperative day. Borderline malignancy IPMN without lymph node metastasis was reported upon the final pathologic examination.
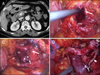
A 74-year-old female patient admitted with abdominal pain for one month. A CT scan and MRI showed an ill-defined mass with multilocular cystic lesion in the body of pancreas. The pancreatic duct was abruptly cut off and the cystic lesion was thought as IPMN accompanied by pancreatic cancer or malignant IPMN of branch duct type (Fig. 3). The preoperative image studies revealed the portal annular pancreas (Fig. 4A). Laparoscopic anterior radical antegrade modular pancreatosplenectomy (RAMPS) was performed. According to the operative findings, portal confluence (SMV-SV-PV) was encased with the uncinate process of pancreas. Therefore, the pancreas needed to be divided twice for a subtotal distal pancreatectomy (Fig. 4B-D). During the postoperative period, grade A postoperative pancreatic fistula occurred, and she was managed with only conservative treatment. She was discharged in good condition on the 16th postoperative day. The pathologic report showed Intraductal papillary mucinous tumor with focal invasive carcinoma transformation.
Pancreas divisum, annular pancreas, and portal annular pancreas are pancreatic fusion anomalies. Pancreas divisum occurs when the fusion of the ventral and dorsal pancreatic buds fails during embryogenesis. This means that two divided pancreas ducts exist to drain pancreatic juice.2 Sometimes this condition causes pancreatitis, because the relatively small orifice of the lesser papilla disrupts drainage of pancreatic juice.3 The annular pancreas surrounds the duodenal second portion completely or incompletely. In this condition, symptoms vary with the degree of duodenal obstruction. A bypass operation such as duodenojejunostomy is needed if there are obstructive symptoms.4 In contrast with annular pancreas, portal annular pancreas completely encasing the PV is asymptomatic in most cases and clinically issued in operative intervention.
Since the first case of portal annular pancreas published by Sugiura et al.5 in 1987, about 10 case reports have been presented. Karasaki et al.6 reported the identification rate of portal annular pancreas to be 1.14%. It is not an extremely rare condition, but may be unrecognized by surgeons. Portal annular pancreas was classified into the suprasplenic, infrasplenic and mixed types according to the level of pancreas fusion.6 Our first case was suprasplenic and the second was a mixed type of portal annular pancreas. This condition is clinically asymptomatic and undetected in most cases. But, it may have clinical significance during certain types of pancreatic surgery, especially pancreatoduodenectomy or subtotal distal pancreatectomy because the pancreas needs to be divided twice around SMV-SV-PV confluence. As mentioned, our two cases required pancreatic division at the pancreatic neck portion twice, which created a potential risk of postoperative pancreatic fistula, as encountered in central pancreatectomy.7 However, most postoperative pancreatic fistulas can be managed in conservative manner. CT scans are useful for the pre-operative detection of portal annular pancreas, and will help to design the operation. Surgeons need to know about this rare pancreatic condition prior to surgical intervention to avoid complications, and to provide patients with well-designed, case-specific pancreatic surgery.
Figures and Tables
Fig. 1
Portal annular pancreas noted in porcine pancreas. The pancreas encased the superior mesenteric vein (SMV) and the portal vein confluence (white arrow).

Fig. 2
Case 1 patient with portal annular pancreas for pancreaticoduodenectomy. The uncinate process of the pancreas encased PV (long white arrow) (A). The multilocular cystic lesion in the uncinate process (arrow head of picture in picture) showed suspicious invasive nature with diffuse soft tissue infiltration around superior mesenteric artery and celiac axis (A). The nP area was dissected from the SMV-PV-SV confluence (B). The uncinate process of the pancreas fused with the dP was divided with endo-GIA (C). The operative field after delivery of the surgical specimen, gastroduodenal artery stump (short white arrow), and division line of uncinate process pancreas (long white arrow) (D).
nP, pancreatic neck; SMV, superior mesenteric vein; PV, portal vein; dP, dorsal pancreas; CHA, common hepatic arery; BD, bile duct.
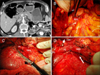
Fig. 3
Preoperative MRI showed an ill-defined mass with multilocular cystic lesion in the body of the pancreas (arrow), suggesting intraductal papillary mucinous neoplasm (IPMN) accompanied by pancreatic cancer or malignant IPMN of branch duct type.
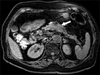
Fig. 4
Case 2 patient with portal annular pancreas for laparoscopic anterior RAMPS. The portal annular pancreas was noted (A). Pancreatic neck dissection for the division. Note the 'pancreatic bridge' between the uncinate process and the doral pancreas (long white arrow) (B). After dividing the pancreatic neck portion, pancreatic fusion was more clearly identified (long white arrow). The SV was also divided at the junction to the SMV (narrow white arrow) (C). Operative field view (D). Besides division of the pancreatic neck portion, an additional pancreatic division line was noted (short white arrow). The origin of the splenic artery (multiple short white arrows) and SV (narrow white arrow) could be observed.
SMV, superior mesenteric vein; SV, splenic vein; CHA, common hepatic artery; PV, portal vein; pP, proximal pancreas; P, pancreas; RAMPS, radical antegrade modular pancreatosplenectomy.
References
1. Truty MJ, Smoot RL. Animal models in pancreatic surgery: a plea for pork. Pancreatology. 2008. 8:546–550.
2. Cotton PB. Congenital anomaly of pancreas divisum as cause of obstructive pain and pancreatitis. Gut. 1980. 21:105–114.
3. Kamisawa T, Tu Y, Egawa N, Tsuruta K, Okamoto A. Clinical implications of incomplete pancreas divisum. JOP. 2006. 7:625–630.
4. Hwang SS, Paik CN, Lee KM, et al. Recurrent acute pancreatitis caused by an annular pancreas in a child. Gastrointest Endosc. 2010. 72:848–849.
5. Sugiura Y, Shima S, Yonekawa H, Yoshizumi Y, Ohtsuka H, Ogata T. The hypertrophic uncinate process of the pancreas wrapping the superior mesenteric vein and artery--a case report. Jpn J Surg. 1987. 17:182–185.
6. Karasaki H, Mizukami Y, Ishizaki A, et al. Portal annular pancreas, a notable pancreatic malformation: frequency, morphology, and implications for pancreatic surgery. Surgery. 2009. 146:515–518.
7. Choi SH, Kang CM, Lee WJ, Chi HS. Robot-assisted spleen-preserving laparoscopic distal pancreatectomy. Ann Surg Oncol. 2011. 18:3623.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download