Abstract
More than 90% cases of chronic gastrointestinal bleeding can be diagnosed by upper endoscopy and/or colonoscopy, and therefore, obscure gastrointestinal bleeding has been defined as bleeding of unknown origin that persists after these conventional endoscopic evaluation. Gastrointestinal stromal tumors (GISTs) are rare tumors, but the most common form of mesenchymal tumors of the gastrointestinal tract. Small bowel is the second most common primary site for GISTs, and accounts for 2-10% of chronic bleeding sites. GISTs usually present as a sporadic and solitary tumor, and a minority of the cases of multiple GISTs are discovered as forms of hereditary or idiopathic tumor syndromes. Small bowel tumor has been difficult to diagnose because of absence of accurate and proper diagnostic tools. Recently developed wireless capsule endoscopy helps in the diagnostic work-up of small bowel diseases. We report a case of multiple jejunal GISTs presenting melena in a 39-year-old male, which was diagnosed with wireless capsule endoscopy.
Figures and Tables
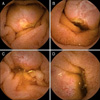 | Fig. 1Capsule endoscopic finding. Luminal protruding masses with central ulcerative lesion were observed at the jejunum, and each lesion is noted at 14 minutes (A), 16 minutes (B), 19 minutes (C), 21 minutes (D) after passage of the pylorus. |
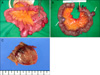
 | Fig. 2Abdominal CT showed multiple exophytic homogeneous enhancing masses with intraluminal central ulcer at the jejunum (arrows). |
 | Fig. 3PET-CT demonstrated several enhancing masses with faint to mild increased fluoro-deoxyglucose (FDG) uptake (SUVmax=2.3) in the small bowel (arrows), and there was no abnormal enlarged lymph node or other lesion with FDG uptake. |
References
1. Leighton JA, Goldstein J, Hirota W, et al. Obscure gastrointestinal bleeding. Gastrointest Endosc. 2003. 58:650–655.
2. Torres M, Matta E, Chinea B, et al. Malignant tumors of the small intestine. J Clin Gastroenterol. 2003. 37:372–380.
3. Galmiche JP, Coron E, Sacher-Huvelin S. Recent developments in capsule endoscopy. Gut. 2008. 57:695–703.
4. Fletcher CD, Berman JJ, Corless C, et al. Diagnosis of gastrointestinal stromal tumors: a consensus approach. Hum Pathol. 2002. 33:459–465.
5. D'Amato G, Steinert DM, McAuliffe JC, Trent JC. Update on the biology and therapy of gastrointestinal stromal tumors. Cancer Control. 2005. 12:44–56.
6. Liu X, Wilcox CM, Nodit L, Lazenby AJ. Multiple gastrointestinal stromal tumors and lipomatosis. Arch Pathol Lab Med. 2008. 132:1825–1829.
7. Raut CP, Morgan JA, Ashley SW. Current issues in gastrointestinal stromal tumors: incidence, molecular biology, and contemporary treatment of localized and advanced disease. Curr Opin Gastroenterol. 2007. 23:149–158.
8. Joensuu H, Fletcher C, Dimitrijevic S, Silberman S, Roberts P, Demetri G. Management of malignant gastrointestinal stromal tumours. Lancet Oncol. 2002. 3:655–664.
9. Demetri GD, Benjamin RS, Blanke CD, et al. NCCN Task Force report: management of patients with gastrointestinal stromal tumor (GIST)--update of the NCCN clinical practice guidelines. J Natl Compr Canc Netw. 2007. 5:Suppl 2. S1–S29.
10. Miettinen M, Makhlouf H, Sobin LH, Lasota J. Gastrointestinal stromal tumors of the jejunum and ileum: a clinicopathologic, immunohistochemical, and molecular genetic study of 906 cases before imatinib with long-term follow-up. Am J Surg Pathol. 2006. 30:477–489.
11. Schwartz GD, Barkin JS. Small-bowel tumors detected by wireless capsule endoscopy. Dig Dis Sci. 2007. 52:1026–1030.
12. Cheung DY, Lee IS, Chang DK, et al. Korean Gut Images Study Group. Capsule endoscopy in small bowel tumors: a multicenter Korean study. J Gastroenterol Hepatol. 2010. 25:1079–1086.
13. Rondonotti E, Pennazio M, Toth E, et al. European Capsule Endoscopy Group. Italian Club for Capsule Endoscopy (CICE). Iberian Group for Capsule Endoscopy. Small-bowel neoplasms in patients undergoing video capsule endoscopy: a multicenter European study. Endoscopy. 2008. 40:488–495.
14. ASGE Standards of Practice Committee. Fisher L, Lee Krinsky M, et al. The role of endoscopy in the management of obscure GI bleeding. Gastrointest Endosc. 2010. 72:471–479.
15. Kang DY, Park CK, Choi JS, et al. Multiple gastrointestinal stromal tumors: Clinicopathologic and genetic analysis of 12 patients. Am J Surg Pathol. 2007. 31:224–232.
16. Díaz-Delgado M, Hernández-Amate A, Sánchez-León M, et al. Multiple non-metastatic gastrointestinal stromal tumors. Differential features. Rev Esp Enferm Dig. 2010. 102:489–497.
17. Hirashima K, Takamori H, Hirota M, et al. Multiple gastrointestinal stromal tumors in neurofibromatosis type 1: report of a case. Surg Today. 2009. 39:979–983.
18. Handra-Luca A, Flejou JF, Molas G, et al. Familial multiple gastrointestinal stromal tumours with associated abnormalities of the myenteric plexus layer and skeinoid fibres. Histopathology. 2001. 39:359–363.
19. Carney JA. Carney triad: a syndrome featuring paraganglionic, adrenocortical, and possibly other endocrine tumors. J Clin Endocrinol Metab. 2009. 94:3656–3662.
20. Pera M, Iglesias M, Puig S, Martínez-Avilés L, Bellosillo B. A sporadic multiple gastrointestinal stromal tumor with unique clinical and molecular features. Hum Pathol. 2011. 42:1194–1199.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download