Abstract
Objective
To develop a model based on non-invasive variables to predict the probability of subsequent maternal and/or neonatal clinical infection in women admitted to hospital for preterm labor with intact membranes.
Methods
Transvaginal ultrasound for measurement of cervical length was performed and maternal blood was collected for the determination of white blood cell (WBC) count at admission in 165 consecutive women with preterm labor (between 20.0 and 35.0 weeks). Clinical infection was defined as the presence of clinical chorioamnionitis at delivery or early onset neonatal sepsis. Receiver operating characteristic (ROC) curves and logistic regression analysis were used for statistical analyses.
Results
The prevalence of clinical infection was 5% (8/165). Women who developed clinical infection had a significantly lower median gestational age at admission, a lower shorter median cervical length, and a higher median WBC count as compared to those who did not develop clinical infection. Logistic regression analysis was performed and a final model was chosen, which included maternal blood WBC, cervical length, and gestational age as the best predictors of clinical infection. A risk score was calculated containing these 3 variables for each patient. The model was shown to have an adequate goodness of fit (P=0.202), and the area under the ROC curve was 0.822, indicating reasonably good discrimination.
Figures and Tables
 | Figure 1Receiver-operator characteristic curves for cervical length (A), white blood cell (B), gestational age (C) in predicting the occurrence of clinical infection. Numbers next to solid dots represent each cutoff value (cervical length: area under the curve 0.721; standard error [SE] 0.068; P=0.030, white blood cell: area under the curve 0.793; SE 0.073; P=0.005, gestational age: area under the curve 0.721; SE 0.076; P=0.035). |
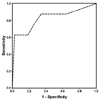 | Figure 2Receiver operator characteristic curve for multivariate prediction model of clinical infection (area under curve 0.822, standard error 0.096, P < 0.002). |
Table 1
Demographic and clinical characteristics of the study population according to the clinical infection

Table 2
Regression coefficients, odds ratios, and 95% confidence intervals of the final model to predict the probability of clinical infection

Formula to predict clinical infection: Y=loge (Z)=-5.694+1.680×[cervical length (mm)>20=0, ≤20=1]+1.767×[WBC count (cells/mm3)<12,600=0, ≥12,600=1]+1.619×[gestational age (weeks)>29=0, ≤29=1].
Z=ey, risk (%)=(Z/1+Z)×100
SE: standard error, CI: confidence interval, WBC: white blood cell, GA: gestational age.
References
1. Mattison DR, Damus K, Fiore E, Petrini J, Alter C. Preterm delivery: a public health perspective. Paediatr Perinat Epidemiol. 2001. 15:Suppl 2. 7–16.

2. Lemons JA, Bauer CR, Oh W, Korones SB, Papile LA, Stoll BJ, et al. Very low birth weight outcomes of the National Institute of Child health and human development neonatal research network, January 1995 through December 1996. NICHD Neonatal Research Network. Pediatrics. 2001. 107:E1.
3. Hillier SL, Krohn MA, Kiviat NB, Watts DH, Eschenbach DA. Microbiologic causes and neonatal outcomes associated with chorioamnion infection. Am J Obstet Gynecol. 1991. 165:955–961.

4. Gomez R, Romero R, Ghezzi F, Yoon BH, Mazor M, Berry SM. The fetal inflammatory response syndrome. Am J Obstet Gynecol. 1998. 179:194–202.

5. Watterberg KL, Demers LM, Scott SM, Murphy S. Chorioamnionitis and early lung inflammation in infants in whom bronchopulmonary dysplasia develops. Pediatrics. 1996. 97:210–215.

6. Yoon BH, Romero R, Park JS, Kim CJ, Kim SH, Choi JH, et al. Fetal exposure to an intra-amniotic inflammation and the development of cerebral palsy at the age of three years. American Journal of Obstetrics and Gynecology. 2000. 182:675–681.

7. Yoon BH, Romero R, Kim CJ, Jun JK, Gomez R, Choi JH, et al. Amniotic fluid interleukin-6: a sensitive test for antenatal diagnosis of acute inflammatory lesions of preterm placenta and prediction of perinatal morbidity. Am J Obstet Gynecol. 1995. 172:960–970.

8. Park KH, Yoon BH, Kim M, Kim GJ, Kim T, Lee HK, et al. A comparative study of the diagnostic value of amniotic fluid interleukin-6 and culture in the antenatal diagnosis of intrauterine infection and prediction of perinatal morbidity in patients with preterm premature rupture of membranes. Korean J Obstet Gynecol. 2000. 43:10.
9. Zalud I, Janas S. Risks of third-trimester amniocentesis. J Reprod Med. 2008. 53:45–48.
10. Gomez R, Romero R, Nien JK, Chaiworapongsa T, Medina L, Kim YM, et al. A short cervix in women with preterm labor and intact membranes: a risk factor for microbial invasion of the amniotic cavity. Am J Obstet Gynecol. 2005. 192:678–689.

11. Holst RM, Jacobsson B, Hagberg H, Wennerholm UB. Cervical length in women in preterm labor with intact membranes: relationship to intra-amniotic inflammation/microbial invasion, cervical inflammation and preterm delivery. Ultrasound Obstet Gynecol. 2006. 28:768–774.

12. Yoon BH, Yang SH, Jun JK, Park KH, Kim CJ, Romero R. Maternal blood C-reactive protein, white blood cell count, and temperature in preterm labor: a comparison with amniotic fluid white blood cell count. Obstet Gynecol. 1996. 87:231–237.

13. Yoon BH, Romero R, Moon JB, Shim SS, Kim M, Kim G, et al. Clinical significance of intra-amniotic inflammation in patients with preterm labor and intact membranes. Am J Obstet Gynecol. 2001. 185:1130–1136.

14. Palacio M, Cobo T, Bosch J, Filella X, Navarro-Sastre A, Ribes A, et al. Cervical length and gestational age at admission as predictors of intra-amniotic inflammation in preterm labor with intact membranes. Ultrasound Obstet Gynecol. 2009. 34:441–447.

15. Watts DH, Krohn MA, Hillier SL, Eschenbach DA. The association of occult amniotic fluid infection with gestational age and neonatal outcome among women in preterm labor. Obstet Gynecol. 1992. 79:351–357.

16. Kayem G, Maillard F, Schmitz T, Jarreau PH, Cabrol D, Breart G, et al. Prediction of clinical infection in women with preterm labour with intact membranes: a score based on ultrasonographic, clinical and biological markers. Eur J Obstet Gynecol Reprod Biol. 2009. 145:36–40.

17. Iams JD, Goldenberg RL, Meis PJ, Mercer BM, Moawad A, Das A, et al. The length of the cervix and the risk of spontaneous premature delivery. National Institute of Child Health and Human Development Maternal Fetal Medicine Unit Network. N Engl J Med. 1996. 334:567–572.
18. Gibbs RS, Romero R, Hillier SL, Eschenbach DA, Sweet RL. A review of premature birth and subclinical infection. Am J Obstet Gynecol. 1992. 166:1515–1528.

19. Smulian JC, Bhandari V, Campbell WA, Rodis JF, Vintzileos AM. Value of umbilical artery and vein levels of interleukin-6 and soluble intracellular adhesion molecule-1 as predictors of neonatal hematologic indices and suspected early sepsis. J Matern Fetal Med. 1997. 6:254–259.

20. Iams JD. The Preterm Prediction Study: cervical length and perinatal infection. Am J Obstet Gynecol. 1997. 176:S6.
21. Romero R, Gonzalez R, Sepulveda W, Brandt F, Ramirez M, Sorokin Y, et al. Infection and labor. VIII. Microbial invasion of the amniotic cavity in patients with suspected cervical incompetence: prevalence and clinical significance. Am J Obstet Gynecol. 1992. 167:1086–1091.
22. Hein M, Valore EV, Helmig RB, Uldbjerg N, Ganz T. Antimicrobial factors in the cervical mucus plug. Am J Obstet Gynecol. 2002. 187:137–144.

23. Lee SE, Romero R, Park CW, Jun JK, Yoon BH. The frequency and significance of intraamniotic inflammation in patients with cervical insufficiency. Am J Obstet Gynecol. 2008. 198:633.

24. Yoon BH, Jun JK, Romero R, Park KH, Gomez R, Choi JH, et al. Amniotic fluid inflammatory cytokines (interleukin-6, interleukin-1beta, and tumor necrosis factor-alpha), neonatal brain white matter lesions, and cerebral palsy. Am J Obstet Gynecol. 1997. 177:19–26.
25. Romero R, Chaiworapongsa T, Espinoza J. Micronutrients and intrauterine infection, preterm birth and the fetal inflammatory response syndrome. J Nutr. 2003. 133:5 Suppl 2. 1668S–1673S.

26. Kenyon SL, Taylor DJ, Tarnow-Mordi W. Broad-spectrum antibiotics for spontaneous preterm labour: the ORACLE II randomised trial. ORACLE Collaborative Group. Lancet. 2001. 357:989–994.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download