The septate uterus, the most common form of structural uterine anomaly, has significant effects on preterm labor, fetal presentation, infertility and spontaneous abortion.1,2 A rare variant of septate uterus, as combined with cervical duplication and a longitudinal vaginal septum, has been anecdotally reported.2-6 Although it is not included in the American Fertility Society classification of müllerian anomalies, it could be successfully treated by excision of the complete longitudinal vaginal septum followed by hysteroscopic septotomy, sparing the double cervix.7,8
The traditional embryologic hypothesis of müllerian development is the fusion of two ducts followed by unidirectional (caudal to cranial) absorption of intervening septum. However, the above mentioned anomalies support the bidirectional theory, i.e., absorption of septum proceeds from uterine isthmus into both directions.6,9
Interesting cases of apparently normal uterus with blinded cervical pouch, dual cervices and complete sagittal vaginal septum were reported.10,11 Similar but unique cases were also reported; the women have a quite normal uterus with a longitudinal vaginal septum and double cervices that communicated at the internal os.12-14 All of these rare müllerian duct anomalies are inconsistent with the classical understanding of linear caudal-to-cephalad fusion. Here we report a case of complete septate uterus with a longitudinal vaginal septum and double cervices that communicated at the lower segment of intervening septum.
Case Report
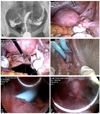
A 30-year-old nulligravid woman was referred to our hospital with 2-year history of primary infertility and suspicious uterovaginal anomaly. She had regular menstrual cycles ranged 30 to 32 days but complained of severe dysmenorrhea. Pelvic examination revealed a longitudinal vaginal septum and two distinct cervices. The hysterosalpingogram was obtained by instillation of contrast medium into the left cervical canal, but the right hemi-uterus could be visualized concomitantly (Fig. 1A). The initial impression was a double uterus with both patent fallopian tubes. In addition, possible communication of both hemi-uteri at the lower segment was firstly suspected.
Further evaluation such as magnetic resonance imaging was not performed. An abdominal ultrasound showed both kidneys present. We decided to perform laparoscopy and concomitant hysteroscopy for the evaluation and correction of the uterovaginal anomaly. Both cervices were ripened by vaginal insertion of 200 µg of prostaglandin E1 (misoprostol) into the left and right vaginal posterior fornix for preparation of hysteroscopy.
Laparoscopic exam revealed a relatively intact uterine fundus with normally located fallopian tubes (Fig. 1B). There was no evidence of uterine didelphys or bicornuate uterus. Periovarian filmy adhesion and moderately obliterated uterosacral ligament was identified and then lysed (Fig. 1C). Several superficial endometriotic foci in the pelvic peritoneum were excised and then coagulated.
Before introduction of hysteroscope, two 14-French Foley catheters were inserted into the uterus through each cervix (Fig. 1D). Hysteroscope was gently inserted into the right cervical canal and confirmed the presence of uterine septation with broad fundal base. Hysteroscopic exam through the right cervix also revealed the Foley catheter inserted through the left cervical canal. Hysteroscopic exam approached into the left cervix also identified the Foley catheter inserted through the right cervix (Fig. 1E). Thus small communication at the lower segment of intervening septum was confirmed. Final hysteroscopic septotomy was performed through the right sided cervix under assistance by laparoscopy and transabdominal sonography (Fig. 1F).
A test of tubal patency using indigocarmine solution confirmed the patency of both fallopian tubes. Finally viscoelastic gel (Gaurdix; Hanmi Pharma, Seoul, Korea) was applied around both uterine adnexa for adhesion prevention. We did not excise the longitudinal vaginal septum because she did not have difficulty in sexual intercourse. Also, we thought it best not to interfere with the following delivery by surgical intervention. The operation took about 100 minutes. The pathologic result of intrauterine septum was reported as proliferative endometrium with small myometrial tissue. Peritoneal biopsy was fibrous tissue with organizing hematoma. Her postoperative course was unremarkable, and she was discharged one day later without any events. We recommended oral cyclic estrogen-progestin for 3 months. After hormone treatment, she is now trying to become pregnant by ovarian stimulation.
DISCUSSION
We described a rare and unique case of complete septate uterus with a longitudinal vaginal septum and double cervices that communicated at the lower segment of intervening septum. Our case was similar to a case of septate bicervical uterus with isthmic communication shown in previous report by Acién et al6; however, a longitudinal vaginal septum was absent in that case report.
Our case could not be classified by traditional caudal-to-cranial müllerian fusion. An alternative embryologic mechanism was hypothesized that fusion occurs at the level of uterine isthmus and simultaneously proceeds in both cranial and caudal directions.9 Midline resorption also begins at the isthmus and is first directed caudally, unifying the cervix and vagina. Our case was unique because it could be hypothesized that the müllerian fusion might be failed in the caudal direction and the septal resorption be failed in the cranial direction, sparing only small portion of intervening septum at the level of uterine isthmus.
Hysteroscopic metroplasty significantly improved the subsequent reproductive outcome for the septate uterus in women with recurrent spontaneous abortion.15 With no metroplasty, prognosis of pregnancy is relatively good in cases of complete septate uterus, but metroplasty can improve the reproductive outcome of complete septate uterus with spontaneous abortion.16
Management of septate uterus in women with otherwise unexplained infertility remains controversial. Previous reports indicate that improvement of pregnancy was modest after hysteroscopic metroplasty in women with septate uterus and otherwise unexplained infertility.1,15 However, there have been several reports regarding negative impact of septum on embryo implantation and improvement of implantation by resection of septum.17-20 Therefore, prophylactic hysteroscopic metroplasty in asymptomatic women is recommended because it may prevent miscarriage or other obstetric complications and to optimize pregnancy outcomes.16 The metroplasty is strongly recommended especially in women with prolonged infertility, in women >35 years old, and in women contemplating assisted reproductive technologies.7
In conclusion, hysteroscopic septotomy under laparoscopy and/or transabdominal sonography is a simple and safe procedure in case of complete septate uterus with a longitudinal vaginal septum and double cervices, irrespective of isthmic communication. The addition of a classification category allowing alternative developmental models should be considered.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download