Abstract
Objective
The purpose of this study was (1) to evaluate the expressions of clusterin, bax, Ki-67, p53, and apoptotic index in epithelial ovarian tumors, borderline and malignant ovarian tumors, (2) to find out the correlation between their expressions and clinicopathological parameters, and (3) to evaluate the effect on the patient's survival according to their expressions.
Methods
The histological and clinical findings of 22 cases of ovarian cystadenomas, 44 cases of borderline tumors and 96 cases of carcinomas were evaluated. Expressions of clusterin, bax, Ki-67, p53, and apoptotic index were studied on paraffin-embedded tissue sections by immunohistochemical methods.
Results
The expressions of clusterin, p53, and Ki-67 were higher in ovarian carcinomas than borderline tumors. The overexpression of p53, and Ki-67 were frequent in high stage, poorly differentiated and bilateral ovarian carcinomas. The overexpressions of clusterin, bax, p53, and Ki-67 showed a statistically significant correlation with histologic type. Apoptotic index was higher in bax overexpression group, but there was no correlation with overexpression of clusterin or p53. Ki-67 was higher in p53 overexpression group, but there was no correlation with overexpression of clusterin or p53. There was no statistically significant correlation with each other between the overexpressions of clusterin, bax, p53, and Ki-67. The overexpressions of clusterin, Ki-67, p53 was associated with overall patient's survival in borderline significance.
Conclusion
The overexpression of p53, and Ki-67 were frequent in poorly differentiated ovarian carcinomas. So the overexpression of p53, and Ki-67 can be used as prognostic factor. The overexpression of clusterin was more in epithelial ovarian carcinomas than in borderline tumors but showed no significant correlation with the overall patient's survival. Further studies are required to clarify the possibility of using clusterin for target therapy in epithelial ovarian carcinomas.
Figures and Tables
 | Figure 1Immunohistochemical staining of clusterin, bax, p53 and Ki-67. (A) Clusterin overexpression in serous cystadenocarcinoma. (B) Bax overexpression in serous cystadenocarcinoma. (C) p53 overexpression (>50%) in serous cystadenocarcinoma. (D) The increased Ki-67 positive cells (>50%) in serous cystadenocarcinoma (×200). |
 | Figure 2Morphology of apoptosis. (A) Apoptoic bodies in serous adenocarcinoma (arrows) (TUNEL method, ×400). (B) Nuclear fragmentation known as apoptotic body in endometrioid adenocarcinoma (arrow head) (TUNEL method, ×600). |
 | Figure 3Kaplan-Meier analysis of overall survival of patients with epithelial ovarian carcinoma according to the overexpressions of (A) Clusterin (P=0.0574), (B) Bax (P=0.7568), (C) Ki-67 (P=0.0591), (D) p53 (P=0.0550), and (E) AI (P=0.8603) (log-rank test). FU: follow up, AI: apoptotic index. |
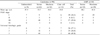
Table 3
Correlation between clinicopathologic characteristics and expressions of clusterin, bax, p53, Ki-67 and AI in epithelial ovarian carcinomas

References
1. Ministry of Health and Welfare. Annual Report of the Korea Central Cancer Registry. 2009. Seoul: Ministry of Health and Welfare.
2. American Cancer Society. Cancer Facts and Figures 2006. 2006. Atlanta: American Cancer Society.
3. Bast RC Jr. Status of tumor markers in ovarian cancer screening. J Clin Oncol. 2003. 21:10 Suppl. 200s–205s.
4. Ozols RF, Rubin SC, Thomas GM, Robboy SJ. Hoskins WJ, Perez CA, Young RC, editors. Epithelial ovarian cancer. Principles and practice of gynecologic oncology. 2000. 3rd ed. Philadelphia: Lippincott Williams and Wilkins;981–1058.
5. Hough CD, Sherman-Baust CA, Pizer ES, Montz FJ, Im DD, Rosenshein NB, et al. Large-scale serial analysis of gene expression reveals genes differentially expressed in ovarian cancer. Cancer Res. 2000. 60:6281–6287.
6. Aronow BJ, Lund SD, Brown TL, Harmony JA, Witte DP. Apolipoprotein J expression at fluid-tissue interfaces: potential role in barrier cytoprotection. Proc Natl Acad Sci U S A. 1993. 90:725–729.
7. Fratelli M, Galli G, Minto M, Pasinetti GM. Role of clusterin in cell adhesion during early phases of programmed cell death in P19 embryonic carcinoma cells. Biochim Biophys Acta. 1996. 1311:71–76.
8. Humphreys DT, Carver JA, Easterbrook-Smith SB, Wilson MR. Clusterin has chaperone-like activity similar to that of small heat shock proteins. J Biol Chem. 1999. 274:6875–6881.
9. Murphy BF, Kirszbaum L, Walker ID, d'Apice AJ. SP-40,40, a newly identified normal human serum protein found in the SC5b-9 complex of complement and in the immune deposits in glomerulonephritis. J Clin Invest. 1988. 81:1858–1864.
10. O'Sullivan J, Whyte L, Drake J, Tenniswood M. Alterations in the post-translational modification and intracellular trafficking of clusterin in MCF-7 cells during apoptosis. Cell Death Differ. 2003. 10:914–927.
11. Parczyk K, Pilarsky C, Rachel U, Koch-Brandt C. Gp80 (clusterin; TRPM-2) mRNA level is enhanced in human renal clear cell carcinomas. J Cancer Res Clin Oncol. 1994. 120:186–188.
12. Steinberg J, Oyasu R, Lang S, Sintich S, Rademaker A, Lee C, et al. Intracellular levels of SGP-2 (Clusterin) correlate with tumor grade in prostate cancer. Clin Cancer Res. 1997. 3:1707–1711.
13. Redondo M, Villar E, Torres-Munoz J, Tellez T, Morell M, Petito CK. Overexpression of clusterin in human breast carcinoma. Am J Pathol. 2000. 157:393–399.
14. Trougakos IP, Gonos ES. Clusterin/apolipoprotein J in human aging and cancer. Int J Biochem Cell Biol. 2002. 34:1430–1448.
15. Sensibar JA, Sutkowski DM, Raffo A, Buttyan R, Griswold MD, Sylvester SR, et al. Prevention of cell death induced by tumor necrosis factor alpha in LNCaP cells by overexpression of sulfated glycoprotein-2 (clusterin). Cancer Res. 1995. 55:2431–2437.
16. Trougakos IP, So A, Jansen B, Gleave ME, Gonos ES. Silencing expression of the clusterin/apolipoprotein j gene in human cancer cells using small interfering RNA induces spontaneous apoptosis, reduced growth ability, and cell sensitization to genotoxic and oxidative stress. Cancer Res. 2004. 64:1834–1842.
17. Wong P, Ulyanova T, Organisciak DT, Bennett S, Lakins J, Arnold JM, et al. Expression of multiple forms of clusterin during light-induced retinal degeneration. Curr Eye Res. 2001. 23:157–165.
18. Leskov KS, Klokov DY, Li J, Kinsella TJ, Boothman DA. Synthesis and functional analyses of nuclear clusterin, a cell death protein. J Biol Chem. 2003. 278:11590–11600.
19. Pucci S, Bonanno E, Pichiorri F, Angeloni C, Spagnoli LG. Modulation of different clusterin isoforms in human colon tumorigenesis. Oncogene. 2004. 23:2298–2304.
20. Xie D, Lau SH, Sham JS, Wu QL, Fang Y, Liang LZ, et al. Up-regulated expression of cytoplasmic clusterin in human ovarian carcinoma. Cancer. 2005. 103:277–283.
21. Kim YJ, Nam DG, Lee JK, Cho SH, Kim KT. P21 and p53 expression in patients with epithelial ovarian carcinoma. Korean J Obstet Gynecol. 2007. 50:1695–1705.
22. Greenblatt MS, Bennett WP, Hollstein M, Harris CC. Mutations in the p53 tumor suppressor gene: clues to cancer etiology and molecular pathogenesis. Cancer Res. 1994. 54:4855–4878.
23. Skilling JS, Sood A, Niemann T, Lager DJ, Buller RE. An abundance of p53 null mutations in ovarian carcinoma. Oncogene. 1996. 13:117–123.
24. Levine AJ, Momand J, Finlay CA. The p53 tumour suppressor gene. Nature. 1991. 351:453–456.
25. Miyashita T, Reed JC. Tumor suppressor p53 is a direct transcriptional activator of the human bax gene. Cell. 1995. 80:293–299.
26. Hermann S, Sturm I, Mrozek A, Klosterhalfen B, Hauptmann S, Dorken B, et al. Bax expression in benign and malignant thyroid tumours: dysregulation of wild-type P53 is associated with a high Bax and P21 expression in thyroid carcinoma. Int J Cancer. 2001. 92:805–811.
27. Sturm I, Papadopoulos S, Hillebrand T, Benter T, Luck HJ, Wolff G, et al. Impaired BAX protein expression in breast cancer: mutational analysis of the BAX and the p53 gene. Int J Cancer. 2000. 87:517–521.
28. Diebold J, Baretton G, Felchner M, Meier W, Dopfer K, Schmidt M, et al. bcl-2 expression, p53 accumulation, and apoptosis in ovarian carcinomas. Am J Clin Pathol. 1996. 105:341–349.
29. Geisler JP, Geisler HE, Wiemann MC, Givens SS, Zhou Z, Miller GA. Quantification of p53 in epithelial ovarian cancer. Gynecol Oncol. 1997. 66:435–438.
30. Henriksen R, Strang P, Wilander E, Backstrom T, Tribukait B, Oberg K. p53 expression in epithelial ovarian neoplasms: relationship to clinical and pathological parameters, Ki-67 expression and flow cytometry. Gynecol Oncol. 1994. 53:301–306.
31. Klemi PJ, Pylkkanen L, Kiilholma P, Kurvinen K, Joensuu H. p53 protein detected by immunohistochemistry as a prognostic factor in patients with epithelial ovarian carcinoma. Cancer. 1995. 76:1201–1208.
32. Levesque MA, Katsaros D, Yu H, Zola P, Sismondi P, Giardina G, et al. Mutant p53 protein overexpression is associated with poor outcome in patients with well or moderately differentiated ovarian carcinoma. Cancer. 1995. 75:1327–1338.
33. Viale G, Maisonneuve P, Bonoldi E, Di Bacco A, Bevilacqua P, Panizzoni GA, et al. The combined evaluation of p53 accumulation and of Ki-67 (MIB1) labelling index provides independent information on overall survival of ovarian carcinoma patients. Ann Oncol. 1997. 8:469–476.
34. Eltabbakh GH, Belinson JL, Kennedy AW, Biscotti CV, Casey G, Tubbs RR, et al. p53 overexpression is not an independent prognostic factor for patients with primary ovarian epithelial cancer. Cancer. 1997. 80:892–898.
35. Hartmann LC, Podratz KC, Keeney GL, Kamel NA, Edmonson JH, Grill JP, et al. Prognostic significance of p53 immunostaining in epithelial ovarian cancer. J Clin Oncol. 1994. 12:64–69.
36. Marks JR, Davidoff AM, Kerns BJ, Humphrey PA, Pence JC, Dodge RK, et al. Overexpression and mutation of p53 in epithelial ovarian cancer. Cancer Res. 1991. 51:2979–2984.
37. Niwa K, Itoh M, Murase T, Morishita S, Itoh N, Mori H, et al. Alteration of p53 gene in ovarian carcinoma: clinicopathological correlation and prognostic significance. Br J Cancer. 1994. 70:1191–1197.
38. Silvestrini R, Daidone MG, Veneroni S, Benini E, Scarfone G, Zanaboni F, et al. The clinical predictivity of biomarkers of stage III-IV epithelial ovarian cancer in a prospective randomized treatment protocol. Cancer. 1998. 82:159–167.
39. Hall PA, Levison DA. Review: assessment of cell proliferation in histological material. J Clin Pathol. 1990. 43:184–192.
40. Biroccio A, D'Angelo C, Jansen B, Gleave ME, Zupi G. Antisense clusterin oligodeoxynucleotides increase the response of HER-2 gene amplified breast cancer cells to Trastuzumab. J Cell Physiol. 2005. 204:463–469.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download