The incidence of Crohn's disease is on the rise. Multi-systemic manifestations of Crohn's disease occur in approximately 35% of patients.1 In patients with Crohn's disease, a higher prevalence of involvement of the anus has been reported (3.8~80%) compared to other inflammatory bowel diseases.2,3 The prevalence of anal disease in Crohn's disease is about 22%, and anal disease should be considered for treatment.4 In Crohn's disease, the anus is affected by abscesses, fistulas, fissures, and strictures, with abscesses and fistulas most common.
A recto-vulva fistula mimics a Bartholin's gland abscess; however, gynecologists are not able to easily differentiate Bartholin's gland abscesses and complications of Crohn's disease. The management of a patient with a Bartholin's gland abscess or recto-vulva fistula complicated by Crohn's disease is very different. The initial management of Crohn's disease of the vulva is medical treatment.
Case Report
A 31-year-old woman (gravida 1, para 1) was admitted to our department at the time with fever before three days. She complained of pain and swelling in the vulva and buttock on the left side. She was treated for Mycobacterium tuberculosis for tuberculosis colitis 5 years previously on her medical history. Two years earlier, she presented with swelling on the left side of the vulva, loose stools, and diarrhea. A colonoscopy confirmed Crohn's disease. After treatment with sulfasalazine, she had complete regression. Three months earlier she had swelling of the left side of the vulva and frequent diarrhea. She had been diagnosed with a Bartholin's gland abscess on the left side of the vulva and underwent marsupialization at the other institution. She developed cellulitis of the left side of buttock as a complication of the Bartholin's gland marsupialization. The gynecologist lost sight of history for Crohn's disease as treated Bartholin's gland abscess. So, three days before she had fever, pain, and swelling from the left side of the vulva to the buttock and admitted.
The vital signs included a blood pressure of 140/100 mm Hg, a pulse rate of 72/minute, a respiratory rate of 20/minute, and a body temperature of 38.2℃. The chest X-ray revealed no abnormal findings. The abdomen was flat and soft with no palpable masses, and no tenderness or rebound tenderness. The genital examination revealed a tender mass on the left side of the vulva and an anal fissure on the right side of the vulva (Fig. 1). There were swelling and discharge on perianal area. The white blood cell count was 3.0×103/µL, and the hemoglobin and hematocrit were 10.5 g/dL, and 31%, respectively. The C-reactive protein was 0.83 mg/dL. The platelet count was 127,000/µL, the PT was 104% (INR 1.12), and the aPTT was 22.7 seconds. The BUN was 8 mg/dL, the creatinine was 0.8 mg/dL, the AST was 14 IU/L, and the APT was 7 IU/L. There were no significant findings on other blood tests, including electrolytes. The urinalysis revealed 1+ leukocytes and grade 4 WBCs (10~29/HPF).
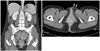
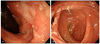
On pelvic computed tomography (CT), a recto-vulva fistula was demonstrated on the right side of the vulva; swelling and edema on the left side of the vulva (Fig. 2). On colonoscopy, we confirmed recurrence of Crohn's disease (Fig. 3). On pelvic examination, a communication between the anal fissure and rectum was demonstrated at 12 o'clock on the external opening of the vulva and 2 cm distance from the anus. The internal opening of the rectum was located 10 o'clock from the anus.
She received antibiotics and sulfasalazine for 7 days. The swelling was relieved. After 7 days of medication, we performed a stricturotomy. Hemostasis was obtained using polyanhydroglucuronic acid (SURGICEL® FIBRILLAR™ Absorbable Hemostat, Johnson & Johnson Ethicon, New Brunswick, NJ, USA). Post-operatively, the symptoms were completely relieved.
Discussion
In a study, there were 55 of 103 patients with Crohn's disease who were misdiagnosed and a large number of these patients had prodromic gynecologic complications.5 Gynecologic complications of Crohn's disease were able to precede active bowel problems and colonoscopic confirmation of Crohn's disease. The gynecologic complication of Crohn's disease was considered an enteric fistula to the vagina, uterus, perineum, vulva, and perianal site.6 Vulva involvement has been reported without active bowel symptoms.7 Fistulas were common, but there were non-ulcerative lesions, such as condylomatous changes.6 Rectovaginal fistulas have been reported at the post-episiotomy site after 1 year.8 Recurrent rectovaginal fistulas of Crohn's disease have been associated with Bartholin's gland carcinoma.9 Long-standing and recurrent Crohn's disease had direct and indirect process to neoplastic condition in vulva.10 So, it is recommended routine physical examination and pelvic examination by gynecologist. This case had fistula on the left side of the vulva. The CT finding and the physical examination in this case were helpful in diagnosing the recto-vulva fistula. Crohn's disease has extra intestinal complication such as fistula, but not easily detected. Magnetic resonance image (MRI) findings revealed incidentally 20% of fistula and abscess.11 CT of abdomen and pelvis showed abscess formation and fistula.12 Perianal complication of Crohn's disease is confuse with Bartholin's gland abscess such as our case. Perianal complication requires full examination of gastrointestinal tract before surgical debridement or fistulotomy. Colostomy and enterostomy with systemic medical treatment are a final method to prevent recurrence.13 We recommend that gynecologists have to obtain a complete history with special attention to gastrointestinal manifestations and remind to diagnose perineal diseases with caution.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download