Abstract
Purpose
To evaluate the medium-term efficacy and safety of transobturator four-arm polypropylene mesh in the treatment of high-stage anterior vaginal wall prolapse and concomitant stress urinary incontinence (SUI).
Materials and Methods
Between September 2010 and August 2013, a prospective single-center trial was performed to evaluate women with stage≥3 anterior vaginal wall prolapse with or without SUI who presented to Labbafinejad Hospital, Teheran, Iran, and underwent anterior vaginal wall repair with polypropylene mesh. Pre- and postoperative evaluation included history; physical examination using the Pelvic Organ Prolapse Quantification system and cough stress test, both before and after reduction of prolapsed structures; Pelvic Floor Distress Inventory (PFDI) and Pelvic Floor Impact Questionnaire (PFIQ); urinalysis and culture; and a postvoid residual assessment. Complications were reported at a mean of 2 years of follow-up.
Results
A total of 71 patients underwent cystocele repair with the transobturator four-arm polypropylene mesh. Seven of the patients were lost to follow-up. There were no perioperative complications. The anatomical success rate was 87.5%. The subjective success rate was 92.1%. The PFDI and PFIQ were significantly improved after surgery (p<0.001). Among those with the simultaneous complaint of SUI, 82% were cured without any additional procedure. Three patients (4.6%) experienced vaginal mesh extrusion. Two patients (3.1%) reported worsening of dyspareunia after surgery.
Pelvic organ prolapse (POP) is a significant worldwide health issue for women [1]. Cystocele or anterior vaginal wall prolapse is the most common type of POP in women [2]. Approaches to the surgical management of POP have undergone several paradigm shifts over the last few decades [3]. The traditional anterior repair of cystocele is associated with a high failure rate, and paravaginal repair is not superior to the traditional anterior repair [1]. Surgical approaches using polypropylene mesh have been widely performed in recent years with high success and low recurrence rates [4].
POP and stress urinary incontinence (SUI) often coexist. There is a controversy regarding the surgical repair of both conditions at the same time. When performed in one session, there is usually a specific procedure for prolapse and another for SUI. After the completion of the cystocele repair, suburethral tape made of polypropylene is placed midurethra, via the transobturator or retropubic route [5].
Synthetic four-arm polypropylene mesh, Nazca-Tc (Promedon, Cordoba, Argentina), was introduced to correct the anterior compartment with the ability to treat SUI at the same time. The mesh has four anchoring arms that facilitate a double transobturator approach for cystocele repair (Fig. 1).
A multicenter trial previously reported a 12-month cure rate of 73% for anterior prolapse by use of this system [6]. The aim of the present prospective single-center trial was to evaluate the safety and efficacy of the four-arm polypropylene mesh (Nazca-Tc) in the treatment of high-stage cystocele and to evaluate clinical outcomes in a subgroup of patients with simultaneous SUI via the double transobturator approach with a mean follow-up of 2 years.
From September 2010 to August 2013, a prospective single-arm study was designed to evaluate the results of the Nazca-Tc (Promedon, Cordoba, Argentina) system in the treatment of high-stage symptomatic cystocele in women. The proposal was approved by the Ethics Committee of the Urology-Nephrology Research Center, Labbafinejad Hospital, Shahid Beheshti University of Medical Sciences, Tehran, Iran, and all patients provided written informed consent. The inclusion criteria were as follows: symptomatic cystocele stage≥3 with or without SUI. Exclusion criteria were active urinary tract or vaginal infection at the time of the operation, evidence of any tearing or severe weakness in the anterior vaginal mucosa, history of previous placement of anterior vaginal wall mesh, or any history or evidence of urogenital malignancies.
Preoperative evaluation consisted of patient history, the Pelvic Floor Distress Inventory short form (PFDI-20), the Pelvic Floor Impact Questionnaire short form (PFIQ-7), physical examination, International Continence Society Pelvic Organ Prolapse Quantification (POP-Q) system [7], and cough stress test, with and without reduction of prolapsed structures. Paraclinical evaluation included urinalysis and culture and measurement of postvoid residual (PVR) urine by bladder ultrasound scan. In cases of severe urinary urgency, urgency incontinence or frequent urinary retention, a multichannel urodynamic study was performed as well. Patients underwent cystocele repair with the Nazca-Tc system.
The procedure was performed with the patient in the lithotomy position under general or spinal anesthesia. A 16-French Foley catheter was inserted through the urethra in the bladder. A midline incision was created in the anterior vaginal wall mucosa from the bladder neck and extended to the cervix (in case of previous hysterectomy, it was extended to the vaginal cuff); wide dissection was carried out laterally to the pelvic sidewalls. The first stab incisions at each side were placed in the anteromedial edge of the obturator foramen at the level of the clitoris, and the proximal incisions were placed 2 cm laterally and 3 cm inferior from the distal incisions. The helical transobturator needles were passed through the groin incision and the obturator space and were then brought to the vaginal cavity. The arms of the mesh were connected to the tip of the needle and brought out through the groin incision.
The central sheet of the mesh was placed underneath the bladder base in a tension-free manner and was sutured at the proximal and distal edges to the cervix and bladder neck by use of 2-0 separate Vicryl sutures. The arms were placed under gentle traction from both sides to adjust the elevation of the bladder. The extra lengths of the arms were cut at the level of the groin incisions. The vaginal mucosa was sutured in an overlying manner by use of 2-0 separate Vicryl sutures. At the end, the mesh was covered by two layers of vaginal mucosa. Vaginal packing was placed and the Foley catheter remained in situ for 12 hours. Concomitant surgeries consisted of sacrospinous ligament fixation by use of the Capio device (Boston Scientific, Natick, MA, USA) in six patients.
Patients presented to follow-up visits at 2 weeks and 1 and 3 months postoperatively and every 6 months thereafter. Objective success was defined as cystocele stage≤1 and a negative result on a cough stress test and subjective success as improvement in the PFDI and PFIQ. Any complications were recorded as well. PFDI and PFIQ scores and PVR were compared pre- and postoperatively by use of paired t-tests.
A total of 71 patients underwent cystocele repair with the Nazca-Tc system via the double transobturator approach. Seven patients were lost to longer follow-up and 64 women had complete follow-up. The patients' mean age was 65.5±8.57 years. Sixty women were postmenopausal (93.7%) without having receiving hormonal replacement therapy. Nineteen (29.6%) and 20 patients (31.2%) had a past medical history of previous cystocele repair by conventional anterior colporrhaphy and abdominal hysterectomy, respectively. None of the patients had any history of previous anti-incontinence surgery (Table 1).
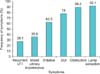
The most common preoperative presenting symptom was the sensation of a lump (92.1%). Other symptoms were obstructive (89.2%) and irritative (62.5%) lower urinary tract symptoms. Thirty-eight and 12 patients (78%) suffered from frank and occult SUI, respectively. Twenty-three patients (35.9%) complained of urinary urge incontinence. Only 18 (28.1%) and 11 patients (17.1%) presented with recurrent urinary tract infection and urinary retention, respectively (Fig. 2).
Cystocele was stages 4 and 3 in 56 (87.5%) and 8 women (12.5%), respectively. Sixty-two women had posterior vaginal wall prolapse (stage 1, 50%; stage 2, 42%; and stage 3, 5%) as well. Only 6 of 64 patients (9.3%) had simultaneous vaginal vault prolapse.
The procedure was uneventful in all patients. Two patients were transfused with one unit of blood postoperatively. Also, two patients complained of pain (groin/pelvic) that required more than 1 week of analgesic treatment. The mean follow-up time was 24 months (range, 10-36 months). The anatomical success rate was 87.5%. Six and two patients had cystocele stages 2 and 3, respectively. The subjective success rate was 92.1%. The PFDI and PFIQ were significantly improved after surgery (p<0.001) (Table 2). Pre- and postoperative mean PVR was 102 cm3 versus 19 cm3 (p<0.001). Postoperative symptoms are listed in Table 3.
Of the 50 patients who complained of SUI, 41 (82%) were cured. One patient with persistent SUI underwent mini-sling surgery at follow-up and was cured postoperatively. Two patients developed de novo SUI.
The mesh exposure rate was 4.6% (3 patients). Two patients were managed with conservative local therapy. One patient underwent revision and partial excision of the exposed part of the mesh.
Only 29 of 64 patients (45.3%) were sexually active at baseline. Of these, 20 patients reported improvement in sexual activity and 7 patients had no change in sexual function. Two patients complained of worsening dyspareunia after surgery.
Recurrent anterior vaginal wall prolapse may develop in more than 20% of patients after native tissue repair [8]. Between 29% and 40% of reconstructive procedures require repeat surgical intervention owing to anatomical failure within 3 years [9]. Of all recurrences, 60% are at the same site, mostly at the anterior compartment [10], whereas 32.5% occur at a different site because of the unmasking of an occult support defect.
Demographic, genetic, and environmental factors have challenged the durability of traditional suture-based native tissue repair and have created the impetus for pelvic reconstructive surgeons to seek the advantages offered by mesh-augmented repair [9]. In 2008, a Cochrane review of the surgical management of POP in women found that placement of a mesh or graft during anterior vaginal wall repair reduces the risk of recurrent prolapse [11]. In the multicenter research clinical trial with the longest follow-up period, Nieminen et al. [12] randomized 105 and 97 women to surgeon-tailored transvaginal mesh and traditional colporrhaphy for anterior vaginal wall prolapse, respectively. At 3 years of follow-up, the authors reported the rates of recurrence of prolapse ≥stage 2 in the POP-Q system to be 13% and 41% in the mesh and traditional repair groups, respectively (p<0.0001). In a prospective study, Moore et al. [1] evaluated 114 women with stage ≥2 anterior vaginal wall prolapse treated with the Perigee system (AMS Inc., Minnetonka, MN, USA) placed via a transobturator route. The clinical success rate at 24 months was 88.5%. Only 10.5% and 4.4% of patients complained of vaginal mesh extrusion and vaginal pain, respectively.
In our study, with a mean of 2 years of follow-up, anatomical and subjective success rates were 87.5% and 92.1%, respectively, which correspond to values in the literature, although with a different commercially available brand.
Advanced POP commonly coexists with SUI. However, in several patients, the SUI may become apparent when the prolapse is corrected. On the other hand, around one-third of patients with either frank or occult SUI experience relief from incontinence after POP repair. Therefore, patients with concomitant POP and SUI pose an additional challenge for surgical repair, involving two procedures at the same time [13]. Generally, for POP accompanied by SUI, there is a specific procedure for prolapse and another for SUI in the treatment strategies, either concomitant or staged. Sergent et al. [14] reported 97% and 81% (69% cure and 12% improvement) success rates for the treatment of cystocele and SUI, respectively, in a single operation by use of the transobturator subvesical mesh repair technique without independent suburethral tape. Palma et al. [6] reported a combined approach, prepubic and transobturator, in the treatment of cystocele and SUI with the Nazca-Tc system. Anterior prolapse and SUI was cured in 73% and 78% of their patients, respectively.
In our study, we used the Nazca-Tc system via the double transobturator route for the treatment of high-stage cystocele resulting in the cure of 82% of the patients with the associated symptom of SUI, without any concomitant procedure for SUI. The results are close to the above-mentioned clinical studies and show that the double transobturator route can address SUI as well as cystocele.
The underlying mechanism of female SUI is reported to be weakness in the supportive mechanisms of the bladder neck or laxity and hypermobility of the midurethra (weakness of the pubourethral ligament). Traditional reconstructive surgeries such as the autologous facial sling technique address the first pathophysiological mechanism and the rationale for the new minimally invasive midurethral tapes such as tension-free vaginal tape and transobturator tape is repair of the second mechanism. In our study, it seems that the positive effect of the double transobturator mesh repair was related to support of the bladder neck, which addresses the first pathophysiologic mechanism.
The most common complication surrounding mesh-augmented repair is exposure of the mesh into the vaginal lumen [9]. Other less common complications are pain (vaginal, groin, buttock, or leg), dyspareunia, mesh contracture, and bladder extrusion [1516]. According to the available randomized controlled trials, the rate of vaginal mesh exposure ranges from 4% to 35.7%. Most erosions are treated under local anesthesia by partial excision, whereas the rest need only topical estrogen. Some cases require full removal [1718192021]. In a recent systematic review, Abed et al. [22] reported an overall erosion rate of 10.3% for the synthetic mesh procedures.
In our study, there was no case of bladder erosion by mesh, whereas the vaginal mesh exposure rate was 4.6% (3 patients). Two of these patients were managed conservatively by application of topical estrogen and only one patient required revision of the exposed part of the mesh. Two patients complained of pain (groin/pelvic).
An important concern with any vaginal repair of organ prolapse is dyspareunia. Recent studies have shown that vaginal mesh does not seem to have a negative impact on sexual function, and prospective comparative studies assessing mesh and traditional repair in the anterior compartment have shown no significant difference in the rate of dyspareunia [232425].
Palma et al. [6] published their results with the Nazca-Tc mesh kit. The rates of mesh exposure, dyspareunia, and de novo enterocele were 4%, 2.7%, and 1.4%, respectively. In our study, 68.9% of patients who were sexually active reported improvement in sexual function after surgery and only 6.8% complained of worsening of dyspareunia.
The limitations of our study included a relatively small number of patients and a single arm rather than a double-arm study design. Also, sexual inactivity in most of our cases prohibits extrapolation of the results. Additional studies with application of the Nazca-Tc system are necessary to evaluate the efficacy and safety of this system.
In this prospective study with a mean of 2 years of follow-up, the Nazca-Tc system was deemed effective and safe in the treatment of advanced anterior vaginal wall prolapse with a low rate of complications after medium-term follow-up. Most of the subgroup with concomitant SUI was cured without a second simultaneous procedure.
Figures and Tables
Table 1
Demographic data

Table 2
Quality of life at 2-year follow-up

Values are presented as mean±standard deviation.
PFDI-20, Pelvic Floor Distress Inventory short form; PFIQ-7, Pelvic Floor Impact Questionnaire short form; POPIQ, Pelvic Organ Prolapse Distress Inventory Questionnaire; UIQ, Urinary Distress Inventory Questionnaire; CRAIQ, Colorectal-Anal Distress Inventory Questionnaire.
References
1. Moore RD, Beyer RD, Jacoby K, Freedman SJ, McCammon KA, Gambla MT. Prospective multicenter trial assessing type I, polypropylene mesh placed via transobturator route for the treatment of anterior vaginal prolapse with 2-year follow-up. Int Urogynecol J. 2010; 21:545–552.
2. Rane A, Iyer J, Kannan K, Corstiaans A. Prospective study of the Perigee™ system for treatment of cystocele - our five-year experience. Aust N Z J Obstet Gynaecol. 2012; 52:28–33.
3. Keys T, Campeau L, Badlani G. Synthetic mesh in the surgical repair of pelvic organ prolapse: current status and future directions. Urology. 2012; 80:237–243.
4. Park HK, Paick SH, Lee BK, Kang MB, Jun KK, Kim HG. Initial experience with concomitant prolift™ system and tension-free vaginal tape procedures in patients with stress urinary incontinence and cystocele. Int Neurourol J. 2010; 14:43–47.
5. Borstad E, Kulseng-Hanssen S, Moghimi K, Sandved M, Majida M, Western K, et al. An incontinence procedure performed at the time of prolapse repair might be unnecessary surgery [Abstract]. Neuroulogy and urodynamics. 2006; 25:551–552. Abstract No. 35
6. Palma P, Riccetto C, Muller V, Rogerio F, Sarsotti C, Ortiz C, et al. Nazca: a monoprosthesis for the simultaneous correction of cystocele and urinary stress incontinence - a multicentric trial. Urology. 2007; 70:Supplement 3A. 193–194.
7. Chapple CR, Milsom I. Urinary incontinence and pelvic prolapse. In : Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA, editors. Campbell-Walsh urology. 10th ed. Philadelphia: Saunders;2012. p. 1900–1903.
8. Handel LN, Frenkl TL, Kim YH. Results of cystocele repair: a comparison of traditional anterior colporrhaphy, polypropylene mesh and porcine dermis. J Urol. 2007; 178:153–156.
9. Lucente V, Murphy M, Saiz C. Vaginal prolapse repair: suture repair versus mesh augmentation: a urogynecology perspective. Urol Clin North Am. 2012; 39:325–333.
10. Clark AL, Gregory T, Smith VJ, Edwards R. Epidemiologic evaluation of reoperation for surgically treated pelvic organ prolapse and urinary incontinence. Am J Obstet Gynecol. 2003; 189:1261–1267.
11. Maher C, Baessler K, Glazener CM, Adams EJ, Hagen S. Surgical management of pelvic organ prolapse in women: a short version Cochrane review. Neurourol Urodyn. 2008; 27:3–12.
12. Nieminen K, Hiltunen R, Takala T, Heiskanen E, Merikari M, Niemi K, et al. Outcomes after anterior vaginal wall repair with mesh: a randomized, controlled trial with a 3 year follow-up. Am J Obstet Gynecol. 2010; 203:235.e1–235.e8.
13. Wu MP, Long CH, Liang CH. Staged or concomitant surgery for correcting pelvic organ prolapse and stress urinary incontinence. Incont Pelvic Floor Dysfunct. 2010; 4:93–98.
14. Sergent F, Sentilhes L, Resch B, Verspyck E, Medeiros R, Descamps P, et al. Treatment of concomitant prolapse and stress urinary incontinence via a transobturator subvesical mesh without independent suburethral tape. Acta Obstet Gynecol Scand. 2010; 89:223–229.
15. Marks BK, Goldman HB. Controversies in the management of mesh-based complications: a urology perspective. Urol Clin North Am. 2012; 39:419–428.
16. Zoorob D, Karram M. Management of mesh complications and vaginal constriction: a urogynecology perspective. Urol Clin North Am. 2012; 39:413–418.
17. Nguyen JN, Burchette RJ. Outcome after anterior vaginal prolapse repair: a randomized controlled trial. Obstet Gynecol. 2008; 111:891–898.
18. Withagen MI, Milani AL, den Boon J, Vervest HA, Vierhout ME. Trocar-guided mesh compared with conventional vaginal repair in recurrent prolapse: a randomized controlled trial. Obstet Gynecol. 2011; 117(2 Pt 1):242–250.
19. Altman D, Vayrynen T, Engh ME, Axelsen S, Falconer C. Nordic Transvaginal Mesh Group. Anterior colporrhaphy versus transvaginal mesh for pelvic-organ prolapse. N Engl J Med. 2011; 364:1826–1836.
20. Vollebregt A, Fischer K, Gietelink D, van der Vaart CH. Primary surgical repair of anterior vaginal prolapse: a randomised trial comparing anatomical and functional outcome between anterior colporrhaphy and trocar-guided transobturator anterior mesh. BJOG. 2011; 118:1518–1527.
21. Lopes ED, Lemos NL, Carramão Sda S, Lunardelli JL, Ruano JM, Aoki T, et al. Transvaginal polypropylene mesh versus sacrospinous ligament fixation for the treatment of uterine prolapse: 1-year follow-up of a randomized controlled trial. Int Urogynecol J. 2010; 21:389–394.
22. Abed H, Rahn DD, Lowenstein L, Balk EM, Clemons JL, Rogers RG, et al. Incidence and management of graft erosion, wound granulation, and dyspareunia following vaginal prolapse repair with graft materials: a systematic review. Int Urogynecol J. 2011; 22:789–798.
23. Sentilhes L, Berthier A, Sergent F, Verspyck E, Descamps P, Marpeau L. Sexual function in women before and after transvaginal mesh repair for pelvic organ prolapse. Int Urogynecol J Pelvic Floor Dysfunct. 2008; 19:763–772.
24. Nieminen K, Hiltunen R, Heiskanen E, Takala T, Niemi K, Merikari M, et al. Symptom resolution and sexual function after anterior vaginal wall repair with or without polypropylene mesh. Int Urogynecol J Pelvic Floor Dysfunct. 2008; 19:1611–1616.
25. Gauruder-Burmester A, Koutouzidou P, Tunn R. Effect of vaginal polypropylene mesh implants on sexual function. Eur J Obstet Gynecol Reprod Biol. 2009; 142:76–80.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download