Abstract
Purpose
The thulium laser is the most recently introduced technology for the surgical treatment of benign prostatic hyperplasia (BPH). Until recently, most thulium laser enucleation of the prostate (ThuLEP) was performed by use of the three-lobe technique. We introduce a novel one-lobe enucleation technique for ThuLEP called the "All-in-One" technique. We report our initial experiences here.
Materials and Methods
From June 2013 to May 2014, a total of 47 patients underwent the All-in-One technique of ThuLEP for symptomatic BPH performed by a single surgeon. All patients were assessed with the International Prostate Symptom Score (IPSS), transrectal ultrasonography, serum prostate-specific antigen (PSA), maximal urine flow rate (Qmax), and postvoid residual urine volume (PVR) before and 1 month after surgery. We reassessed IPSS, Qmax, and PVR 3 months after surgery. To assess the efficacy of the All-in-One technique, we checked the PSA reduction ratio, transitional zone volume reduction ratio, and enucleation failure rate.
Results
The mean operative time was 82.1±33.3 minutes. The mean enucleation time and morcellation time were 52.7±21.7 minutes and 8.2±7.0 minutes, respectively. The mean resected tissue weight and decrease in hemoglobin were 36.9±24.6 g and 0.4±0.8 g/dL, respectively. All perioperative parameters showed significant improvement (p<0.05). No major complications were observed. The PSA reduction ratio, transitional zone volume reduction ratio, and enucleation failure rate were 0.81, 0.92, and 4.3%, respectively.
In aging males, benign prostatic hyperplasia (BPH) is one of the most common and bothersome diseases influencing quality of life [1]. For decades, transurethral resection of the prostate (TURP) has been recognized as the standard treatment for BPH [2]. In recent years, laser treatment of BPH has challenged TURP as the result of advances in laser technology, better understanding of tissue-laser interactions, and growing clinical experience [3]. Although green light laser photoselective vaporization has been proved to be a safe and effective surgical procedure comparable to TURP, photoselective vaporization has the limitations of providing no tissue specimen for histological evaluation and having a significantly slower speed of tissue ablation [4]. According to the results of recent randomized studies, holmium laser enucleation of the prostate (HoLEP) can be applied to all cases of BPH regardless of prostate size and has been proved to be an alternative to TURP or open prostatectomy [56]. The most beneficial aspect of HoLEP may be an enucleation function similar to that of open prostatectomy.
The recently introduced thulium laser has a wavelength similar to that of the holmium laser but has been found to be superior in spatial beam quality, precise incision, and wave continuity [7]. In comparative studies, thulium laser enucleation of the prostate (ThuLEP) showed results comparable to those of HoLEP [89].
In this study, we introduce a new one-lobe enucleation technique of ThuLEP. We call it the "All-in-One" technique. We predicted that the technique might even better reproduce the enucleation ability of open prostatectomy. We report our initial results here.
From June 2013 to May 2014, a total of 47 symptomatic BPH patients who underwent the All-in-One technique of ThuLEP were evaluated. We analyzed the patients' medical records retrospectively. Inclusion criteria were as follows: maximal urine flow rate (Qmax) less than 15 mL/s or postvoid residual urine volume (PVR) above 50 mL or repeated urinary retention or lower urinary tract symptoms with an International Prostate Symptom Score (IPSS) above 7. Patients with prostate cancer, urethral stricture, or a previous history of urologic surgery were excluded.
All surgeries were performed by a single surgeon. All patients were assessed with medical history, digital rectal examination (DRE), IPSS, transrectal ultrasonography (TRUS), serum prostate-specific antigen (PSA), Qmax, and PVR before surgery and 1 month after surgery. Three months after surgery, we reassessed IPSS, Qmax, and PVR. Perioperative data (i.e., operative time, enucleation time, morcellation time, resected tissue weight, serum hemoglobin decrease, catheterization day, postoperative complications) were recorded. To evaluate enucleation efficacy, we assessed the PSA reduction ratio ([preoperative PSA level-postoperative PSA level]/[preoperative PSA level]), transitional zone volume reduction ratio (resected tissue weight/preoperative transitional zone volume), and enucleation failure rate. Enucleation failure was defined as cases in which postoperative TRUS revealed remnant adenoma in the transitional zone.
In patients who had risk factors for prostate cancer (e.g., PSA value above 4 ng/mL, nodule on DRE, or hypoechoic lesion on TRUS), prostate biopsy was performed to rule out cancer. Patients who proved to have prostate cancer through preoperative biopsy or postoperative biopsy were also excluded.
We analyzed the mean values of parameters with paired Student t-test. The significance level was defined as a p-value <0.05.
The instruments used were a 70-W continuous-wave Tm:yttrium aluminium garnet laser (Revolix, LISA Laser Products OHG, Katlenburg-Lindau, Germany) and a 26-French continuous flow resectoscope (Richard Wolf Medical Instruments, Vernon Hills, IL, USA). The enucleated prostatic tissues were morcellated by use of a Piranha morcellator (Richard Wolf Medical Instruments, Vernon Hills, IL, USA). Saline irrigation was applied to all cases. Laser energy was set to 40 W during all procedures.
The surgical steps of the All-in-One technique of ThuLEP are follows. An overview is shown in Supplementary material (video clip).
Enucleation begins at the apex. An inverted-U-shaped incision around the verumontanum is made (Fig. 1A). The incision is continued until the surgical capsule is identified. After inspection of the urethral sphincter, a marking incision is made at 12 o'clock at the apex to ensure the safety of the sphincter (Fig. 1B). Then the superior 12 o'clock incision line and the end of the inverted-U-shaped incision line at inferior 5 and 7 o'clock are connected circumferentially (Fig. 1C).
After confirming the safety of the urethral sphincter once more, a deep incision is made along the lateral circumferential line until the surgical capsule is visible starting from 5 or 7 o'clock to 12 o'clock. If the circumferential surgical capsule is wholly identified, the enucleation process goes on to the bladder neck along the obtained circumferential surgical capsule with use of the thulium laser for the incision and coagulation and the beak of the resectoscope for blunt dissection. Near the bladder neck, freeing of the enucleated prostatic adenoma proceeds from 12 o'clock in a latero-inferior direction. The 5 to 7 o'clock area, the median lobe, is freed last (Fig. 1D).
After freeing of the entire prostatic lobe circumferentially from the surgical capsule, the last step before morcellation is to ensure that there is no significant bleeding. If there is no significant bleeding, the morcellator is then inserted into the bladder to morcellate the enucleated prostatic adenoma.
A total of 47 patients who underwent the All-in-One ThuLEP technique were included in this study. Mean patient age was 69.8±7.4 years. Mean operative time was 82.1±33.3 minutes, mean enucleation time was 52.7±21.7 minutes, mean morcellation time was 8.2±7.0 minutes, mean resected tissue weight was 36.9±24.6 g, mean hemoglobin decrease was 0.4±0.8 g/dL, and mean number of catheterization days was 2.8±2.0 days (Table 1).
Preoperative mean TRUS prostate volume and mean transitional zone volume were 66.9±38.6 cm3 and 40.6±26.4 cm3, respectively. Mean PSA was 7.8±15.9 ng/mL, mean IPSS was 24.8±7.9, mean Qmax was 7.3±4.5 mL/s, and mean PVR volume was 137.6±201.0 mL.
All patients were followed up 1 month and 3 months after surgery. After 1 month, mean TRUS prostate volume was 11.7±10.0 cm3, mean transitional zone volume was 0.9±4.8 cm3, mean PSA was 0.5±0.4 ng/mL, mean IPSS was 17.5±10.0, mean Qmax was 15.6±7.8 mL/s, and mean PVR was 30.0±20.7 mL. After 3 months, mean IPSS was 11.5±7.1, mean Qmax was 15.8±9.0 mL/s, and mean PVR was 27.3±17.5 mL. All 1-month follow-up values were significantly improved over the corresponding preoperative values (p<0.05). The 3-month follow-up IPSS was significantly improved compared with the 1-month follow-up score (p<0.05). Neither Qmax nor PVR showed significant changes at 3 months (Table 2).
The PSA reduction ratio was 0.81±0.23 and the transitional zone volume reduction ratio was 0.92±0.34. There were only 2 cases of enucleation failure; the enucleation failure rate was 4.3% (Table 3).
Perioperative complications are shown in Table 4. No cases required blood transfusion. There were also no cases of capsular perforation, ureteral orifice injury, or urinary tract infection. Two cases of superficial bladder injury occurred while performing morcellation (4.3%), and there were 8 cases of temporary urinary retention (17.0%), 1 case of stress urinary incontinence (2.1%), and 1 case of urethral stricture. All patients with temporary urinary retention improved after 1 week of Foley catheterization. Stress urinary incontinence subsided within 1 month after surgery. There were no significant complications.
Prostate enucleation with a laser is a safe, effective, and minimally invasive technique regardless of prostate size, and recent studies have reported that it can substitute for TURP or open prostatectomy [310]. In particular, both thulium and holmium lasers have high efficacy and safety in relieving the lower urinary tract symptoms of BPH patients [89].
During the past 2 decades, holmium laser surgery for BPH has gradually advanced in the fields of both laser technology and surgical techniques. In the 1990s, holmium laser ablation and resection of the prostate was introduced. Since the introduction of the tissue morcellator, holmium laser ablation and resection has largely been superseded by HoLEP [3]. HoLEP was first reported in 1998 by Gilling et al. [11]. Since then many studies have reported promising results that support the excellency of HoLEP for BPH surgery. To date, many surgeons have adapted the 'three-lobe' technique for HoLEP. To facilitate enucleation, Krambeck et al. [12] and Baazeem et al. [13] proposed a two-lobe technique. To further improve surgical effectiveness, trials of technical modifications have continued.
Similar to the holmium laser, the thulium laser works with a wavelength of 2013 nm, which can be easily absorbed into water, especially interstitial water. The waves of the thulium laser are more continuous than those of the holmium laser and therefore provide more effective hemostasis. In addition, it provides accurate resection with sufficient vaporization, and the moving laser probe maximizes vaporization but reduces the heat applied to tissue [14].
The development of thulium laser prostate surgery has proceeded very similarly to that of holmium laser surgery. Four different techniques have been described so far: thulium vaporization of the prostate, thulium vaporesection (ThuVaRP), thulium vapoenucleation (ThuVEP), and thulium enucleation (ThuLEP). ThuVaRP was initially reported in 2005 by Xia et al. [15]. They introduced the prostate-tangerine technique and reported its safety and efficacy. We also reported a comparative study of ThuVaRP and TURP. The results showed that ThuVaRP had the same therapeutic effect as TURP and had the advantages of a shorter hospital stay and shorter catheter indwelling time. However, ThuVaRP had a limitation in that the operation time took longer as the prostate size increased. Thus, ThuVaRP is more suitable for a relatively small prostate [16]. To overcome the prolonged operation time in a large prostate, Bach et al. [17] reported the technique of ThuVEP, and its functional outcomes were comparable with those of HoLEP. Also, there was no limitation in prostate size. ThuLEP was introduced in 2010 by Herrmann et al. [18]. They said that ThuLEP offers the opportunity for maximum removal of obstruction of the prostate urethra similar to open prostatectomy but with maximum control of hemostasis.
As mentioned above, the surgical techniques of the holmium and thulium laser have been developed to reproduce and resemble the enucleation techniques of open prostatectomy. It is expected that greater tissue removal will result in better functional results with regard to improvement of Qmax, PVR, and the re-treatment rate. Our All-in-One technique can mostly reproduce the enucleation techniques of open prostatectomy.
We expect that this new technique may have three advantages over the usual two- or three-lobe technique: shortening the operation time, reducing blood loss, and improving the effectiveness of enucleation. However, these advantages were not proven in the present study because this was a preliminary study and contains our initial experience. Theoretically, however, we can reduce the incision and dissecting surface, and the possibility of encountering unexpected bleeding can be lowered because the 5 or 7 o'clock incision from the apex to the bladder neck of the ordinary technique is not needed in the All-in-One technique. In this study, we reported comparable results. The mean enucleation time was 52.7 minutes and the mean hemoglobin decrease was 0.4 g/dL. Also, there was no transfusion. To evaluate enucleation efficacy, we used three parameters: PSA reduction ratio, transitional zone volume reduction ratio, and enucleation failure rate. The PSA reduction ratio was 0.81, which was comparable to previously reported ThuLEP or HoLEP results [18]. There are no other reports that used the transitional zone volume reduction ratio (0.92) and the enucleation failure rate (4.3%) as the parameters for assessing enucleation efficacy. We think that both parameters can best reflect how well enucleation is performed.
Although more long-term data and well-designed comparative study are needed, our initial results of the All-in-One technique are promising. We believe that the All-in-One technique for ThuLEP will be the most effective surgical management for BPH.
We introduce a novel one-lobe technique of ThuLEP, the All-in-One technique, and report its initial results. Our initial results prove that the All-in-One technique is not inferior to another technique for symptomatic BPH surgery and is a feasible and promising technique. Future well-designed comparative study and long-term data can prove that this new technique has some advantages in terms of operation time, hemostasis, and enucleation efficacy.
Figures and Tables
Fig. 1
Overview of 'All-in-One' technique. (A) Making an inverted-U shaped incision line. (B) Marking incision at 12 o'clock area of apex. (C) Connecting the incision line circumferentially. (D) Enucleation. Scan this QR code to see the accompanying video, or visit www.kjurology.org or https://youtu.be/ShJ6GLAR2MY.


Table 1
Perioperative data

Table 2
Perioperative changes of clinical parameters

Values are presented as mean±standard deviation.
TRUS, transrectal ultrasound; NA, not analyzed; T-zone, transitional zone; PSA, prostate-specific antigen; IPSS, International Prostate Symptom Score; Qmax, maximal urine flow rate; PVR, postvoid residual urine volume.
a:p-value comparing preoperative and 1-month parameters. b:p-value comparing 1-month and 3-month parameters.
Table 3
Parameters of enucleation efficacy
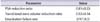
| Parameter | Value |
|---|---|
| PSA reduction ratio | 0.81±0.23 |
| Transitional zone volume reduction ratio | 0.92±0.34 |
| Enucleation failure rate | 2/47 (4.3) |
Table 4
Complications

References
1. Berry SJ, Coffey DS, Walsh PC, Ewing LL. The development of human benign prostatic hyperplasia with age. J Urol. 1984; 132:474–479.
2. Wasson JH, Reda DJ, Bruskewitz RC, Elinson J, Keller AM, Henderson WG. A comparison of transurethral surgery with watchful waiting for moderate symptoms of benign prostatic hyperplasia. The Veterans Affairs Cooperative Study Group on Transurethral Resection of the Prostate. N Engl J Med. 1995; 332:75–79.
3. Gravas S, Bachmann A, Reich O, Roehrborn CG, Gilling PJ, De La Rosette J. Critical review of lasers in benign prostatic hyperplasia (BPH). BJU Int. 2011; 107:1030–1043.
4. Ruszat R, Seitz M, Wyler SF, Abe C, Rieken M, Reich O, et al. GreenLight laser vaporization of the prostate: single-center experience and long-term results after 500 procedures. Eur Urol. 2008; 54:893–901.
5. Gilling PJ, Wilson LC, King CJ, Westenberg AM, Frampton CM, Fraundorfer MR. Long-term results of a randomized trial comparing holmium laser enucleation of the prostate and transurethral resection of the prostate: results at 7 years. BJU Int. 2012; 109:408–411.
6. Chen YB, Chen Q, Wang Z, Peng YB, Ma LM, Zheng DC, et al. A prospective, randomized clinical trial comparing plasmakinetic resection of the prostate with holmium laser enucleation of the prostate based on a 2-year follow-up. J Urol. 2013; 189:217–222.
7. Fried NM, Murray KE. High-power thulium fiber laser ablation of urinary tissues at 1.94 microm. J Endourol. 2005; 19:25–31.
8. Zhang F, Shao Q, Herrmann TR, Tian Y, Zhang Y. Thulium laser versus holmium laser transurethral enucleation of the prostate: 18-month follow-up data of a single center. Urology. 2012; 79:869–874.
9. Hong K, Liu YQ, Lu J, Xiao CL, Huang Y, Ma LL. Efficacy and safety of 120-W thulium:yttrium-aluminum-garnet vapoenucleation of prostates compared with holmium laser enucleation of prostates for benign prostatic hyperplasia. Chin Med J (Engl). 2015; 128:884–889.
10. Herrmann TR, Liatsikos EN, Nagele U, Traxer O, Merseburger AS. EAU Guidelines Panel on Lasers, Technologies. EAU guidelines on laser technologies. Eur Urol. 2012; 61:783–795.
11. Gilling PJ, Kennett K, Das AK, Thompson D, Fraundorfer MR. Holmium laser enucleation of the prostate (HoLEP) combined with transurethral tissue morcellation: an update on the early clinical experience. J Endourol. 1998; 12:457–459.
12. Krambeck AE, Handa SE, Lingeman JE. Experience with more than 1,000 holmium laser prostate enucleations for benign prostatic hyperplasia. J Urol. 2010; 183:1105–1109.
13. Baazeem AS, Elmansy HM, Elhilali MM. Holmium laser enucleation of the prostate: modified technical aspects. BJU Int. 2010; 105:584–585.
14. Bach T, Herrmann TR, Ganzer R, Burchardt M, Gross AJ. RevoLix vaporesection of the prostate: initial results of 54 patients with a 1-year follow-up. World J Urol. 2007; 25:257–262.
15. Xia SJ, Zhang YN, Lu J, Sun XW, Zhang J, Zhu YY, et al. Thulium laser resection of prostate-tangerine technique in treatment of benign prostate hyperplasia. Zhonghua Yi Xue Za Zhi. 2005; 85:3225–3228.
16. Kim JW, Kim YJ, Lee YH, Kwon JB, Cho SR, Kim JS. An Analytical comparison of short-term effectiveness and safety between thulium:YAG laser vaporesection of the prostate and bipolar transurethral resection of the prostate in patients with benign prostatic hyperplasia. Korean J Urol. 2014; 55:41–46.
17. Bach T, Wendt-Nordahl G, Michel MS, Herrmann TR, Gross AJ. Feasibility and efficacy of Thulium:YAG laser enucleation (VapoEnucleation) of the prostate. World J Urol. 2009; 27:541–545.
18. Herrmann TR, Bach T, Imkamp F, Georgiou A, Burchardt M, Oelke M, et al. Thulium laser enucleation of the prostate (ThuLEP): transurethral anatomical prostatectomy with laser support. Introduction of a novel technique for the treatment of benign prostatic obstruction. World J Urol. 2010; 28:45–51.
SUPPLEMENTARY MATERIAL
An accompanying video can be found in the 'urology in motion' section of the journal homepage (www.kjurology.org). The supplementary video clips can also be accessed by scanning a QR code located on the Fig. 1 of this article, or be available on YouTube (http://youtu.be/ShJ6GLAR2MY).




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download