Abstract
Purpose
To evaluate the distribution of ureteral stones and to determine their characteristics and expulsion rate based on their location.
Materials and Methods
We retrospectively reviewed computed tomography (CT) findings of 246 patients who visited our Emergency Department (ED) for renal colic caused by unilateral ureteral stones between January 2013 and April 2014. Histograms were constructed to plot the distribution of stones based on initial CT findings. Data from 144 of the 246 patients who underwent medical expulsive therapy (MET) for 2 weeks were analyzed to evaluate the factors responsible for the stone distribution and expulsion.
Results
The upper ureter and ureterovesical junction (UVJ) were 2 peak locations at which stones initially lodged. Stones lodged at the upper ureter and ureteropelvic junction (group A) had a larger longitudinal diameter (4.21 mm vs. 3.56 mm, p=0.004) compared to those lodged at the lower ureter and UVJ (group B). The expulsion rate was 75.6% and 94.9% in groups A and B, respectively. There was no significant difference in the time interval from initiation of renal colic to arrival at the ED between groups A and B (p=0.422). Stone diameter was a significant predictor of MET failure (odds ratio [OR], 1.795; p=0.005) but the initial stone location was not (OR, 0.299; p=0.082).
The global prevalence of urinary stones has been estimated to be between 2% and 20% and has risen during the last 2 decades. Approximately 20% of all urinary stones occur in the ureter [123]. In general, diagnoses of ureteral stones mainly depend on comprehensive physical examination and radiological imaging studies, including kidney-ureter-bladder (KUB) films, intravenous urography (IVU), and computed tomography (CT) scan [4]. Due to high sensitivity and specificity in identifying urinary stones, CT scan has become the gold standard for diagnosing ureteral stones [456].
Quick and accurate assessment of stone characteristics is extremely important because such information determines treatment modalities. Notably, identifying exact stone locations increases success rates and reduces treatment time. It has been known during several decades that ureteral stones impact at 3 narrowing sites: the ureteropelvic junction (UPJ), ureteral crossing of the iliac vessels (CUIV), and ureterovesical junction (UVJ) [67]. In clinical practice, however, ureteral stone location does not always correspond to the narrowing sites of the ureter as currently known. Previous studies have proposed that the CUIV may not be one of the main locations at which urinary stones lodge as assessed using IVU. However, such imaging studies are inaccurate in identifying exact urinary tract structures because there are anatomical differences among individuals [78].
This study evaluated the exact location of ureteral stones using CT scan and determined their characteristics and expulsion rates according to the peak stone locations.
We retrospectively reviewed the medical records of 246 patients who visited our Emergency Department (ED) for renal colic and were diagnosed with a single unilateral ureteral stone under 10 mm in maximum diameter using CT between January 2013 and April 2014. Histograms were constructed to plot the distribution of stones based on initial CT findings of the total cohort (n=246).
Of the 246 patients, 144 who met the following criteria were selected for further analysis to investigate the effect of initial stone location on the success of medical expulsive therapy (MET). Inclusion criteria were (1) revisit to the Department of Urology for follow-up, (2) MET with tamsulosin 0.2 mg for at least 2 weeks, and (3) stones located at the peak distribution sites based on the histograms. Patients with past history of active treatment such as ureteroscopic surgery, laparoscopic surgery, or extracorporeal shockwave lithotripsy for ureteral stone were excluded from the study. All the patients were offered with MET as an initial treatment modality unless the patients had febrile urinary tract infection or intolerable pain that cannot be controlled with oral analgesics. Patients received tamsulosin at a daily oral dose of 0.2 mg for 2 weeks. Stone expulsion was defined as the absence of ureteral stones on CT scans or KUB films taken 2 weeks after MET. Patients were categorized into 2 groups according to stone location: those who had stones in the upper ureter and UPJ (group A, n=45) and those who had stones in the lower ureter and UVJ (group B, n=99).
Axial and coronal CT scans were obtained and analyzed by 2 independent urologists (H.J.K. and Y.J.M.). The size of ureteral stones was measured by the largest diameter on CT scan. Stone locations were classified as the UPJ, upper ureter (between the renal pelvis and the upper border of the sacrum), the midureter (above the iliac vessels), the mid ureter (below the iliac vessels), the lower ureter (between the lower border of the sacrum and the ureterovesical junction), UVJ, and ureteral orifice.
All data were analyzed using IBM SPSS Statistics ver. 20.0 (IBM Co., Armonk, NY, USA). Differences in the characteristics of urinary stones were evaluated using the chi-square test for nonparametric variables, and Student t-test and the Mann-Whitney U test for parametric variables. Binary logistic regression was used to analyze predictors of MET failure. A p-value of less than 0.05 was considered statistically significant.
In total cohort (n=246), the mean age of the patients was 46.04α14.15 years. The male to female ratio was 159 (64.6%) to 87 (35.4%). Thirty patients (18.8%) had a history of ipsilateral ureteral stones, and 15 patients (9.4%) were conservatively managed. Stones were situated on the left side in 116 patients (47.2%) and on the right side in 130 patients (52.8%). The median stone diameter was 3.98 mm (interquartile range, 3.08-5.68). The upper ureter (37.0%) and UVJ (36.2%) were the 2 peak locations at which the stones initially lodged (Fig. 1).
Of the selected subjects who underwent MET for 2 weeks (n=144), the stone diameter was larger in group A than in group B (4.21 mm vs. 3.56 mm, p=0.004) (Table 1). There were no significant differences in the previous stone history between groups A and B (6.8% vs 7.1%, p=0.956). The stone expulsion rates were 75.6% and 94.9% in groups A and B, respectively. There were no significant differences in the time interval from initiation of renal colic to arrival at the ED between groups A and B (2.0 hours vs. 1.5 hours, p=0.422).
Even though stones tended to have a higher expulsion failure rate in group A than in group B (OR, 0.299; p=0.087), only stone diameter was a significant predictor of MET failure in subjects with stone size 10mm or less (OR, 1.795; p=0.005) (Table 2).
The standard diagnostic tool to detect urinary stones has shifted from IVU to CT due to higher sensitivity and specificity [9]. This shift is induced by the introduction of low-dose CT, which has diagnostic value with relatively low radiation dosage compared to the standard CT [1011]. As the anatomy of the ureter and adjacent structures is accurately evaluated by CT scans, there is accumulating evidence that clinicians have incorrect information on urinary stone location.
When IVU was the main tool for diagnosing ureter stone, the UPJ, CUIV, and UVJ were considered as the narrowing sites of the ureter where the stones lodge. There is an abrupt reduction in the internal caliber of the ureter at the UPJ and UVJ where the renal pelvis tapers into the upper ureter, lower ureter, and then bladder wall. Nevertheless, the CUIV is different from the aforementioned 2 anatomical sites in that the CUIV is caused by the extrinsic compression of the iliac vessels but not the intrinsic change in the ureter, which is supported by the results of a study by Song et al. [2] that the CUIV is not significantly narrower than other parts of the ureter.
Discrepancies in stone locations have stimulated researchers to explore exact lodging sites in order to confirm that the traditional treatment is incorrect. Ordon et al. [7] identified 2 peaks in stone distribution as the UPJ/upper ureter and intramural ureter/UVJ by reviewing KUB films of 622 patients with a solitary ureteral stone referred for SWL. They also categorized the stone location into 19 sites referenced to the axial skeleton on CT scans. The limitation of their study is that only 12% of patients had both noncontrast CT scans and KUB films. Identifying stone only with KUB can be inaccurate because there are anatomical variations among individuals. To overcome this limitation, we only retrieved data from patients who were diagnosed with ureteral stones using CT. We also failed to demonstrate a peak in stone distribution corresponding to the CUIV.
Even though most studies, including ours, support the concept that there is no peak stone distribution in the CUIV, a few argue that the initial location of ureteral stones detected on imaging studies is not the final one. To identify the final stone location, we investigated at which stones are situated in patients who failed 2 weeks of MET. Of the 246 patients, 11 (24.4%) in group A and 5 (5.1%) in group B had failed MET. Most of these 16 patients (13 out of 16) showed the same location, except for 3 patients in group A whose stones migrated downward to finally lodge at the lower ureter/UVJ, not at the CUIV. Ordon et al. [7] reported stone distribution in patients with ureteral stones referred for SWL. The stone distribution in the ureter is consistent with ours. Similar stone distribution despite such time gap supports that CUIV is not a temporary but not final point at which stones lodge.
We compared the characteristics of stones situated at the 2 peak locations. Previous studies have shown that stone size is a most powerful single predictor that affects stone location [61213]. Consistent with results of previous studies, smaller stones were more likely to lodge at the lower part of the ureter [14]. In most studies, patients with a previous history of stones were excluded. In our study, however, we included patients with prior history of ipsilateral ureteral stones that were nonsurgically managed. We demonstrated that the initial location of the stones was not a significant predictor of MET failure at 2 weeks after MET (OR, 0.299; p=0.087) (Table 2). To find out whether MET failure is influenced by a previous history of active treatment on the same side of ureter, subjects who fulfill all other inclusion criteria except for a previous history of SWL or ureteroscopic stone removal for ipsilateral ureteral stones were added to the MET cohort for additional analysis. In this patient group (n=156), stone diameter (OR, 1.689; p=0.008) and initial stone location (OR, 6.973; p=0.003) were significant predictors of MET failure (data not shown). This suggests that patients who have undergone active treatment may have strictures in the ureter which probably require a longer time for the ureteral stones to be spontaneously expelled and have a higher possibility of undergoing additional treatment other than MET.
This study has some limitations. First, there is a possible selection bias owing to the retrospective design of the study. Patients were not adequately followed up with a precise protocol, and some of them were lost to follow-up. Second, the sample size of this study was small. Third, this study provided insufficient information on factors that may affect stone expulsion, such as use of calcium channel blockers in patients with hypertension or the amount of daily fluid intake.
The results of this study suggest that the upper ureter and UVJ could be 2 peaks in stone distribution except for the CUIV. Nevertheless, for stone size 10 mm or less, initial stone lodge site is not a significant predictor of MET failure in patients who have no prior history of treatment for ipsilateral ureteral stones.
Figures and Tables
Fig. 1
The locations of ureteral stones in the anatomical portions of the ureter in 246 patients (total cohort). UPJ, ureteropelvic junction; UVJ, ureterovesical junction.
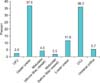
Table 1
Comparison of the stone characteristics between the ureter stones that lodged at UPJ/upper ureter and lower ureter/UVJ

Table 2
Predictive factors for medical expulsive treatment failure within 2 weeks after renal colic caused by unilateral ureteral stone using binary logistic regression

ACKNOWLEDGMENTS
We are grateful to Physician Assistants Eun Suk Park and Jung Kyoung Kim for their help with data collection.
References
1. Stamatelou KK, Francis ME, Jones CA, Nyberg LM, Curhan GC. Time trends in reported prevalence of kidney stones in the United States: 1976-1994. Kidney Int. 2003; 63:1817–1823.
2. Song HJ, Cho ST, Kim KK. Investigation of the location of the ureteral stone and diameter of the ureter in patients with renal colic. Korean J Urol. 2010; 51:198–201.
3. Ketabchi AA, Mehrabi S. The effect of tamsulosin, an alpha-1 receptor antagonist as a medical expelling agent in success rate of ureteroscopic lithotripsy. Nephrourol Mon. 2013; 6:e12836.
4. Chua ME, Gomez OR, Sapno LD, Lim SL, Morales ML Jr. Use of computed tomography scout film and Hounsfield unit of computed tomography scan in predicting the radio-opacity of urinary calculi in plain kidney, ureter and bladder radiographs. Urol Ann. 2014; 6:218–223.
5. Ryu JA, Kim B, Jeon YH, Lee J, Lee JW, Jeon SS, et al. Unenhanced spiral CT in acute ureteral colic: a replacement for excretory urography? Korean J Radiol. 2001; 2:14–20.
6. El-Barky E, Ali Y, Sahsah M, Terra AA, Kehinde EO. Site of impaction of ureteric calculi requiring surgical intervention. Urolithiasis. 2014; 42:67–73.
7. Ordon M, Schuler TD, Ghiculete D, Pace KT, Honey RJ. Stones lodge at three sites of anatomic narrowing in the ureter: clinical fact or fiction? J Endourol. 2013; 27:270–276.
8. Eisner BH, Reese A, Sheth S, Stoller ML. Ureteral stone location at emergency room presentation with colic. J Urol. 2009; 182:165–168.
9. Bader MJ, Eisner B, Porpiglia F, Preminger GM, Tiselius HG. Contemporary management of ureteral stones. Eur Urol. 2012; 61:764–772.
10. Jellison FC, Smith JC, Heldt JP, Spengler NM, Nicolay LI, Ruckle HC, et al. Effect of low dose radiation computerized tomography protocols on distal ureteral calculus detection. J Urol. 2009; 182:2762–2767.
11. Park SH, Kim KD, Moon YT, Myung SC, Kim TH, Chang IH, et al. Pilot study of low-dose nonenhanced computed tomography with iterative reconstruction for diagnosis of urinary stones. Korean J Urol. 2014; 55:581–586.
12. Eisner BH, Pedro R, Namasivayam S, Kambadakone A, Sahani DV, Dretler SP, et al. Differences in stone size and ureteral dilation between obstructing proximal and distal ureteral calculi. Urology. 2008; 72:517–520.
13. Coll DM, Varanelli MJ, Smith RC. Relationship of spontaneous passage of ureteral calculi to stone size and location as revealed by unenhanced helical CT. AJR Am J Roentgenol. 2002; 178:101–103.
14. Hubner WA, Irby P, Stoller ML. Natural history and current concepts for the treatment of small ureteral calculi. Eur Urol. 1993; 24:172–176.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download