Abstract
Purpose
To investigate the efficacy of androgen deprivation treatment (ADT) between continuous and intermittent ADT.
Materials and Methods
Between January 2006 and May 2015, 603 patients were selected and divided into continuous ADT (CADT) (n=175) and intermittent ADT (IADT) (n=428) groups. The median follow-up in this study was 48.19 (1.0-114.0) months. The primary end point was time to castration resistant prostate cancer (CRPC). The types of ADT were monotherapy and maximal androgen blockade (i.e., luteinizing hormone-releasing hormone agonist and antiandrogen).
Results
The characteristics of patients showed no significant differences between the CADT and IADT groups, except for the Gleason score (p<0.001). The median time to CRPC of all enrolled patients with ADT was 20.60±1.60 months. The median time to CRPC was 11.20±1.31 months in the CADT group as compared with 22.60±2.08 months in the IADT group. In multivariate analysis, percentage of positive core (p=0.047; hazard ratio [HR], 0.976; 95% confidence interval [CI], 0.953-1.000), Gleason score (p=0.007; HR, 1.977; 95% CI, 1.206-3.240), lymph node metastasis (p=0.030; HR, 0.498; 95% CI, 0.265-0.936), bone metastasis (p=0.028; HR, 1.921; 95% CI, 1.072-3.445), and CADT vs. IADT (p=0.003; HR, 0.254; 95% CI. 0.102-0.633) were correlated with the duration of progression to CRPC. The IADT group presented a significantly longer median time to CRPC compared with the CADT group. Additionally, patients in the IADT group showed a longer duration in median time to CRPC in subgroup analysis according to the Gleason score.
Prostate cancer is one of the most commonly diagnosed cancers in the male population [1]. Since Huggins and Hodges demonstrated the responsiveness of prostate cancer to androgen deprivation therapy (ADT), it has become the foundation in managing locally advanced or recurrent prostate cancer patients [2]. At present, ADT is considered one of the most effective therapies for treatment of these patients. There are two kinds of methods used in this therapy: continuous ADT (CADT) and intermittent ADT (IADT). There have been some controversies over the efficacy and adverse events associated with these two methods.
Although CADT had been the standard treatment, IADT has been suggested as an alternative therapy since the 1990s. Additionally, IADT has been recently recommended as the first-line hormonal therapy for advanced prostate cancer patients by the European Association of Urology (EAU) [3]. However, the effect of IADT as compared with CADT still remains ambiguous.
Some studies have suggested that IADT was less effective than CADT in the median time to castration resistant prostate cancer (CRPC), while other studies indicate that IADT is not inferior to CADT. In recent years, there have been several accounts that point to the beneficial effects of IADT when compared with CADT.
Therefore, we compared the effects of IADT and CADT treatment and investigated the relative factors contributing to the median time to CRPC. The aim of this study was to compare the efficacy of IADT and CADT, with an emphasis on the advantages of IADT. Moreover, we investigated relevant factors (age, body mass index [BMI], bone metastasis, clinical T stage, the type of method, prior definite treatment, prostate-specific antigen [PSA] before ADT, Gleason score, and lymph node metastasis) that affect the time to CRPC.
This study included 603 prostate adenocarcinoma patients diagnosed by prostate biopsy from 800 patients who received ADT in a single center from 2006 to 2015. The study was retrospectively analyzed and divided into two therapeutic groups: CADT and IADT groups. We fix on a date that the date was May 2015.
In the CADT group, the previous ADT continued until the disease progressed or the study ended. In the IADT group, ADT was paused when PSA had reached a nadir below 1 ng/mL; it was promptly reintroduced when the PSA level exceeded 4 ng/mL or whenever relative symptoms developed. If the PSA level exceeded 4 ng/mL during an off-period, the patient visited the hospital to restart the ADT. The IADT group was categorized into on-period and off-period subgroups according to the physician's discretion. The on-period was defined as starting from the date of the first injection of the cycle until the date after the last ADT injection of the cycle. The off-period was defined as starting from the date after the last injection until the date of the next injection.
All patients measured PSA level, before starting the ADT. The period of induction was from 3 to 6 months, and PSA levels were measured 3, 6, 12, 18, 24, 30, and 36 months after starting the treatment in the outpatient clinic. When a patient visited, data regarding the patient's clinical symptoms, discomfort, and tolerance to treatment were collected, and laboratory blood tests were carried out (i.e., white and red blood cells counts, and hemoglobin, testosterone, estrogen, liver, and renal function tests). In both groups, radiologic examinations [4] (i.e., abdomen computed tomography [CT], chest CT, and bone scans) were performed before ADT and during the ADT. The efficacy endpoint included CRPC state; this was assessed according to the definition set by the EAU.
The statistical analysis was conducted using IBM SPSS Statistics ver. 20.0 (IBM Co., Armonk, NY, USA) utilizing Student t-test and chi-square test. Statistical significance was examined and defined as p-values less than 0.05. log-rank test was applied to compare groups with respect to median time to CRPC, Correction for the different covariates and risk factors that affected median time to CRPC was evaluated by Cox proportional hazard model. All study protocols were approved by the medical ethics commission of the Institutional Review Board, Pusan National University Hospital. Informed consent was obtained from all patients before enrollment in the study and after explaining the purpose and methods.
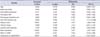
Between January 2006 and May 2015, 603 patients underwent ADT; one group (n=175) underwent CADT, and another group (n=428) underwent IADT. The average median follow-up period was 48.19 (1.0-114.0) months. There were no significant differences between the two groups in age, BMI, PSA before ADT, positive core percent, definite treatments before ADT (prostatectomy or radiotherapy), the clinical T stage of patents, bone metastasis, or lymph node metastasis (p=0.059, p=0.289, p=0.798, p=0.665, p=0.481, p=0.079, p=0.207, and p=0.129), respectively. The definite treatments before ADT were composed of radiotherapy, operation, both radiotherapy and operation. In IADT vs. CADT group, the percentage of patients with radiotherapy, operation, both radiotherapy and operation were 15.3% vs. 22.4%, 3.8% vs. 2.1%, and 2.2% vs. 0%. Only the Gleason score showed meaningful differences in chi-square tests (Table 1). In this study, the incidence rate of CRPC in all patients was 27.4% (197 of 603).
According to univariate analyses, age (p=0.044), PSA before ADT (p=0.001), percentage of positive core (p=0.003), Gleason score (p<0.001), clinical T stage (p=0.008), bone metastasis (p<0.001), and types of method (CADT or IADT, p<0.001) were significant factors related to median time to CRPC.
In multivariate analyses, there was a significant positive correlation between percentage of positive core (p=0.047), Gleason score (p=0.007), lymph node metastasis (p=0.030), bone metastasis (p=0.028), and type of method (p=0.003). From these analyses, we were able to deduct that the difference of method is the most influential factor affecting median time to CRPC. All factors affecting the time to CRPC are shown in Table 2. The median time to CRPC of all enrolled patients after initiation of ADT was 20.60±1.60 months. The median time to CRPC was 11.20±1.31 months in the CADT group as compared with 22.60±2.08 months in the IADT group, representing a 0.25 relative increase in the risk of CRPC with IADT. There was a statistically significant difference in treatment efficacy between the CADT and IADT groups (p<0.001) (Fig. 1). Therefore, we tentatively concluded that IADT was superior to CADT with respect to median time to CRPC.
Because the Gleason score was the meaningful effective factor, we further analyzed according to Gleason scores using Kaplan-Meier analysis. We were split into two groups (low and intermediate Gleason scores vs. high Gleason score) according to the extent of the Gleason score. The median time to CRPC of patients with low and intermediate Gleason scores was 14.90±4.90 months in the CADT group, as compared with 33.47±4.31 months in the IADT group (Fig. 2A). The median time to CRPC of patients with high Gleason score was 10.07±0.07 months in the CADT group, as compared with 20.50±0.50 months in the IADT group (Fig. 2B). There were no significant differences in median time to CRPC of patients with low and intermediate Gleason scores (p=0.194). However, there was a significant difference in median time to CRPC of patients with high Gleason scores (p=0.039).
ADT has become the first-line treatment for advanced prostate cancer, either locally advanced or metastatic beyond the prostate and nearby tissues, into lymph nodes, bones, and other organs in the body. Furthermore, ADT has a symptomatic and/or objective response in approximately 80% of patients [56]. ADT is composed of CADT and IADT. Hormonal therapy is typically continuous and maintained until the progression of the disease, or the patient dies. IADT has been suggested as a feasible treatment option for select patients with prostate cancer. In IADT, patients are treated cyclically with hormonal therapy plus an off-therapy time. For each cycle, ADT is maintained until the PSA becomes undetectable or a nadir level is reached. Then patients are observed without treatment. Patients restart treatment if their PSA increases, or if any objective evidence of disease progression is shown in radiologic images such as x-ray, CT, or bone scans [7].
CADT has been regarded as a standard therapy in locally advanced or recurrent prostate cancer; however, this method has shown some weaknesses. One of the disadvantages of CADT is that it can cause metabolic syndrome due to androgen deficiency. The decrease in hormone levels induced by ADT can cause adverse effects. The adverse effects of ADT are immediate and obvious in some cases and insidious in others. ADT had a variety of well recognized adverse effects such as vasomotor flushing, reduced or absent libido, fatigue, gynecomastia, anemia, osteoporosis, erectile dysfunction, decreased mental acuity, loss of muscle mass, weight gain, depression and increased risk of cardiovascular disease and diabetes [89]. IADT has various appealing points: reduced adverse events, improved quality of life, decreased costs, and perhaps prolonged median time to CRPC. Among them, duration of median time to CRPC has been highly controversial.
Some authors have reported that, in comparison to CADT, IADT has many advantages in terms of reducing adverse events and improving quality of life. In the South European Uroncological Group 9401 trial [10], the patients on IADT experienced lower incidence of hot flashes, fewer problems related to sexual function, and increased sexual activity (p<0.01). The risk of dying from cardiovascular disease increased with the use of CADT (cardiovascular deaths: 41 [13.1%] in the IADT group; 52 [16.7%] in the CADT group). Additionally, many studies, report that quality of life improves during the off-period in IADT [11121314]. On the other hand, in the TULP trial [15], there was no clinically significant difference in quality of life or sexual dysfunction between CADT and IADT groups. Many other studies also report no significant differences in quality of life [1216]. Thus, there has been much debate over whether IADT is superior to CADT in improving quality of life and reducing adverse effects. In the past, median time to CRPC using IADT was inferior to CADT, but nowadays, several randomized phase III trials have proposed that IADT is associated with similar efficacy to that of CADT regarding progression and overall survival [11121718]. In addition, The EAU recently acknowledged that IADT should no longer be considered an experimental therapy [1]. Along with this, we found that IADT showed a longer duration of the median time to CRPC than CADT. In many studies regarding the median time to CRPC, IADT is reported to have similar or less efficacy than that of CADT. However, in the current study, the efficacy of IADT was far better than that of CADT and this result was statistically significant.
An important strength of our study is that there were no significant differences between the characteristics of patients in both the CADT and IADT groups except for the Gleason score. Moreover, we could maintain homogeneity because patients were treated by a single surgeon. In spite of these strengths, there are some limitations in our study. First, the sample size of the CADT group was too small compared to the IADT group (n=175 vs. n=428). This was inevitable since this study was not a random control trial but rather a retrospective study. Second, most of the patients in the CADT group were in the initial stages of treatment; therefore, these patients more rapidly progressed to CRPC compared with patients in the IADT group. Despite this, the study's findings are still meaningful.
Due to these limitations, there may have been a selection bias in the design of this study.
Before ADT, there were significance differences in patients' Gleason scores; therefore we analyzed the Gleason scores and found statistically significant differences between groups. One group was composed of patients with low and intermediate Gleason scores, while another group was composed of patients with high Gleason scores. This is because there were very few patients with low Gleason scores (CADT group, n=18; vs. IADT group, n=84). Although there were no significant differences in low and intermediate Gleason scores, there were significant differences in patients with high Gleason scores.
Figures and Tables
Fig. 1
Comparison of efficacy between continuous ADT and intermittent ADT group in all patients. CRPC, castration resistant prostate cancer; ADT, androgen deprivation treatment.
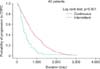
Fig. 2
Comparison of efficacy between continuous ADT and intermittent ADT group in patients. (A) Low and intermittent Gleason score, (B) high Gleason score. CRPC, castration resistant prostate cancer; ADT, androgen deprivation treatment.

Table 1
Patients' characteristics in continuous and intermittent ADT group

Table 2
Factors affecting the time to CRPC in univariate and multivariate analysis
ACKNOWLEDGMENTS
This work was supported by clinical research grant from Pusan National University Hospital 2015.
References
1. Heidenreich A, Bastian PJ, Bellmunt J, Bolla M, Joniau S, van der Kwast T, et al. EAU guidelines on prostate cancer. part 1: screening, diagnosis, and local treatment with curative intent-update 2013. Eur Urol. 2014; 65:124–137.
2. Schroder F, Crawford ED, Axcrona K, Payne H, Keane TE. Androgen deprivation therapy: past, present and future. BJU Int. 2012; 109:Suppl 6. 1–12.
3. Heidenreich A, Aus G, Bolla M, Joniau S, Matveev VB, Schmid HP, et al. EAU guidelines on prostate cancer. Eur Urol. 2008; 53:68–80.
4. Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009; 45:228–247.
5. Lepor H, Shore ND. LHRH Agonists for the treatment of prostate cancer: 2012. Rev Urol. 2012; 14:1–12.
6. Denis L, Murphy GP. Overview of phase III trials on combined androgen treatment in patients with metastatic prostate cancer. Cancer. 1993; 72:12 Suppl. 3888–3895.
7. Conti PD, Atallah AN, Arruda H, Soares BG, El Dib RP, Wilt TJ. Intermittent versus continuous androgen suppression for prostatic cancer. Cochrane Database Syst Rev. 2007; (4):CD005009.
8. Saylor PJ, Smith MR. Metabolic complications of androgen deprivation therapy for prostate cancer. J Urol. 2013; 189:1 Suppl. S34–S42.
9. Sharifi N, Gulley JL, Dahut WL. An update on androgen deprivation therapy for prostate cancer. Endocr Relat Cancer. 2010; 17:R305–R315.
10. Calais da Silva FE, Bono AV, Whelan P, Brausi M, Marques Queimadelos A, Martin JA, et al. Intermittent androgen deprivation for locally advanced and metastatic prostate cancer: results from a randomised phase 3 study of the South European Uroncological Group. Eur Urol. 2009; 55:1269–1277.
11. Tunn UW, Canepa G, Kochanowsky A, Kienle E. Testosterone recovery in the off-treatment time in prostate cancer patients undergoing intermittent androgen deprivation therapy. Prostate Cancer Prostatic Dis. 2012; 15:296–302.
12. Crook JM, O'Callaghan CJ, Duncan G, Dearnaley DP, Higano CS, Horwitz EM, et al. Intermittent androgen suppression forrising PSA level after radiotherapy. N Engl J Med. 2012; 367:895–903.
13. Salonen AJ, Taari K, Ala-Opas M, Viitanen J, Lundstedt S, Tammela TL, et al. Advanced prostate cancer treated with intermittent or continuous androgen deprivation in the randomised FinnProstate Study VII: quality of life and adverse effects. Eur Urol. 2013; 63:111–120.
14. Salonen AJ, Taari K, Ala-Opas M, Viitanen J, Lundstedt S, Tammela TL, et al. The FinnProstate Study VII: intermittent versus continuous androgen deprivation in patients with advanced prostate cancer. J Urol. 2012; 187:2074–2081.
15. Langenhuijsen JF, Badhauser D, Schaaf B, Kiemeney LA, Witjes JA, Mulders PF. Continuous vs. intermittent androgen deprivation therapy for metastatic prostate cancer. Urol Oncol. 2013; 31:549–556.
16. Irani J, Celhay O, Hubert J, Bladou F, Ragni E, Trape G, et al. Continuous versus six months a year maximal androgen blockade in the management of prostate cancer: a randomised study. Eur Urol. 2008; 54:382–391.
17. Calais da Silva F, Calais da Silva FM, Gonçalves F, Santos A, Kliment J, Whelan P, et al. Locally advanced and metastatic prostate cancer treated with intermittent androgen monotherapy or maximal androgen blockade: results from a randomised phase 3 study by the South European Uroncological Group. Eur Urol. 2014; 66:232–239.
18. Mottet N, Van Damme J, Loulidi S, Russel C, Leitenberger A, Wolff JM, et al. Intermittent hormonal therapy in the treatment of metastatic prostate cancer: a randomized trial. BJU Int. 2012; 110:1262–1269.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download